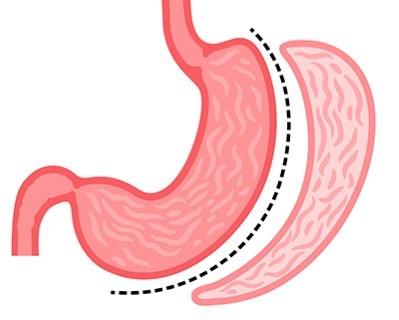
Sleeve Gastrectomy
- Purpose: Reduces the size of the stomach to limit food intake and promote weight loss.
- Procedure: A large portion of the stomach is removed, creating a sleeve-shaped stomach.
-
Note: The information provided here applies to elective Sleeve Gastrectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of obesity-related comorbidities, patient tolerance, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Sleeve Gastrectomy is typically performed as an inpatient procedure. This major weight-loss surgery requires patients to be admitted to the hospital for close monitoring before, during, and after the procedure. Most patients will require a hospital stay to ensure proper recovery and to monitor for any potential complications, such as bleeding, infection, or nutrient deficiencies.Hospital Stay Duration
Patients undergoing Sleeve Gastrectomy usually stay in the hospital for 2 to 3 days. The initial post-operative period involves monitoring in a specialized care unit to observe for any complications and to manage pain and recovery. The length of stay may be extended if the patient has other underlying conditions or if complications arise during recovery.Type of Anesthesia
The procedure is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. General anesthesia is necessary to keep the patient comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after Sleeve Gastrectomy surgery. This period allows time for initial recovery and healing. The healthcare provider will provide specific recommendations regarding travel and activity levels based on the patient’s recovery progress.Pre-procedure Preparation
Preparation for Sleeve Gastrectomy typically involves several steps, including dietary adjustments, weight loss, and lifestyle changes to optimize health before surgery. Patients are usually instructed to follow a liquid or low-calorie diet for a few weeks before surgery to reduce the size of the liver and improve surgical outcomes. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during surgery. A comprehensive pre-operative assessment, including blood tests and imaging studies, is conducted to plan the surgery.Procedure Duration
The Sleeve Gastrectomy procedure typically takes 1 to 2 hours. The surgery involves removing approximately 75-80% of the stomach, leaving a tube-shaped stomach or "sleeve." This significantly reduces the stomach's capacity, leading to reduced food intake and promoting weight loss.Recovery Time
Recovery from Sleeve Gastrectomy surgery can take several weeks. Most patients are encouraged to engage in light activities, such as walking, soon after discharge, but full recovery, including a return to work and more strenuous activities, may take up to 4 to 6 weeks. Patients will need to follow a special diet, starting with liquids and gradually progressing to pureed and then solid foods. Regular follow-up appointments and participation in a bariatric surgery support program are essential for monitoring weight loss progress and addressing any nutritional needs or complications.Estimated Cost
The cost of Sleeve Gastrectomy surgery can vary widely depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for Sleeve Gastrectomy involves a significant focus on diet and lifestyle changes. Patients will need to follow a structured eating plan, including taking vitamin and mineral supplements to prevent deficiencies. Regular follow-up appointments are crucial to monitor weight loss, nutritional status, and any potential complications. Patients will also receive guidance on incorporating physical activity into their routine to support long-term weight loss and health. Psychological support or counseling may be recommended to help patients adjust to the changes following surgery and to address any emotional or behavioral issues related to eating.
_20240708122007087317__0.webp)