Gynecology And Obstetrics Treatments
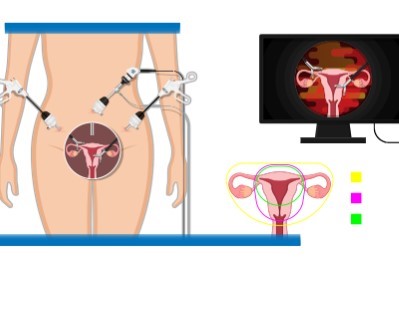
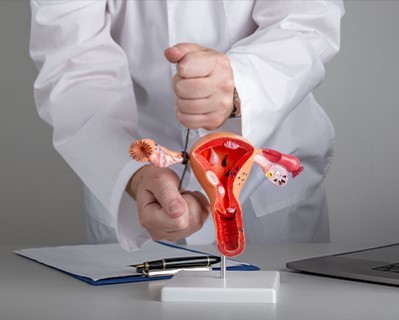
Laparoscopic Hysterectomy
- Purpose: Removes the uterus to treat conditions such as fibroids, endometriosis, and uterine cancer.
- Procedure: The uterus is removed using minimally invasive laparoscopic techniques.
-
Note: The information provided here applies to standard Laparoscopic Hysterectomy procedures under typical conditions. However, specifics may vary based on individual factors such as the patient’s overall health, the complexity of the surgery, and any complications that might arise during or after the procedure. Patients seeking this procedure through health tourism should also consider local regulations and the importance of selecting a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Laparoscopic hysterectomy is usually performed as an inpatient procedure, with most patients requiring a short hospital stay for observation and initial recovery.Hospital Stay Duration
Patients typically stay in the hospital for 1 to 2 days after a laparoscopic hysterectomy. This allows for monitoring, pain management, and ensuring that the patient is stable before discharge.Type of Anesthesia
The procedure is performed under general anesthesia, ensuring the patient is fully unconscious and pain-free during the surgery.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 2 to 4 weeks after the procedure to allow for proper healing and to monitor for any potential complications such as infection or bleeding.Pre-procedure Preparation
Preparation for a laparoscopic hysterectomy involves following specific instructions from the healthcare provider, such as fasting before surgery, adjusting medications, and undergoing pre-operative tests like blood work and imaging. Patients should also ensure they have all necessary documentation and medical records if traveling internationally for the procedure.Procedure Duration
The laparoscopic hysterectomy procedure typically lasts between 1 to 3 hours, depending on the complexity of the surgery. The surgeon uses small incisions and specialized instruments to remove the uterus, often employing a laparoscope for visual guidance.Recovery Time
Recovery from a laparoscopic hysterectomy is generally quicker than from traditional open surgery. Most patients can resume light activities within 1 to 2 weeks, but full recovery may take 4 to 6 weeks. It’s important to avoid heavy lifting and strenuous activities during the recovery period.Estimated Cost
The cost of a laparoscopic hysterectomy can vary depending on factors such as the surgeon's expertise, the complexity of the procedure, and the geographic location of the surgery. Patients should consult their healthcare provider or hospital for detailed cost information, including any additional fees for medications and follow-up care.Post-procedure Care
Post-operative care for a laparoscopic hysterectomy includes managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions for wound care, activity restrictions, and gradually returning to normal activities. Follow-up appointments are important to monitor recovery and address any concerns. Any signs of complications, such as increased pain, fever, or unusual discharge, should be reported to the healthcare provider immediately.
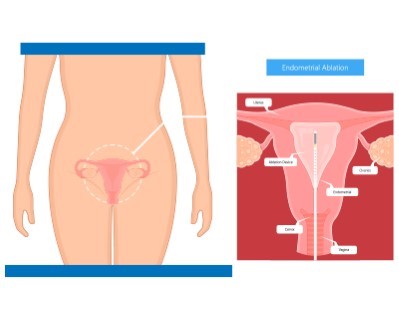
Endometrial Ablation
- Purpose: Treats heavy menstrual bleeding by destroying the lining of the uterus.
- Procedure: Various methods, including heat, cold, or radiofrequency, are used to ablate the endometrium.
-
Note: The information provided here applies to standard Endometrial Ablation procedures under typical conditions. However, specifics may vary based on individual factors, such as the patient’s overall health, the type of ablation method used, and any complications that might arise during or after the procedure. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Endometrial ablation is typically performed as an outpatient procedure, allowing most patients to return home the same day after a brief recovery period.Hospital Stay Duration
Patients undergoing endometrial ablation generally do not require an overnight hospital stay. They are usually discharged a few hours after the procedure, once they have recovered from anesthesia and are stable.Type of Anesthesia
Endometrial ablation is usually performed under local or regional anesthesia, though general anesthesia may be used depending on the patient’s condition and the specific technique employed.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 24 to 48 hours after the procedure to allow for initial recovery and to monitor for any potential complications, such as cramping or bleeding.Pre-procedure Preparation
Preparation for endometrial ablation involves following specific instructions from the healthcare provider, which may include fasting before surgery, adjusting medications, and undergoing pre-operative tests such as blood work and imaging. Patients should ensure they have all necessary documentation and medical records if traveling internationally for the procedure.Procedure Duration
The endometrial ablation procedure typically lasts between 30 minutes to 1 hour, depending on the method used. The surgeon uses various techniques, such as heat, cold, or radiofrequency energy, to destroy the lining of the uterus to reduce or stop menstrual bleeding.Recovery Time
Recovery from endometrial ablation is generally quick, with most patients able to resume light activities within a few days. Full recovery may take about 1 to 2 weeks. Patients should avoid strenuous activities and sexual intercourse until cleared by their healthcare provider.Estimated Cost
The cost of endometrial ablation can vary depending on the method used, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and medications.Post-procedure Care
Post-operative care for endometrial ablation includes managing pain, preventing infection, and monitoring for any signs of complications. Patients may experience cramping, mild pain, or watery discharge for a few days after the procedure. Follow-up appointments are essential to ensure proper healing and to discuss the results of the procedure. Any signs of complications, such as heavy bleeding, fever, or severe pain, should be reported to the healthcare provider immediately.

Hysteroscopy
- Purpose: Diagnoses and treats problems within the uterus, such as polyps, fibroids, and abnormal bleeding.
- Procedure: A hysteroscope is inserted through the vagina and cervix to examine and treat the uterus.
-
Note: The information provided here applies to standard Hysteroscopy procedures under typical conditions. However, specifics may vary based on individual factors, such as the patient’s overall health, the purpose of the hysteroscopy, and any complications that might arise during or after the procedure. Patients seeking this procedure through health tourism should also consider local regulations and the importance of selecting a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Hysteroscopy is typically performed as an outpatient procedure, allowing most patients to return home the same day after a short recovery period.Hospital Stay Duration
Patients undergoing hysteroscopy generally do not require an overnight hospital stay. They are usually discharged a few hours after the procedure, once they have recovered from anesthesia and are stable.Type of Anesthesia
Hysteroscopy can be performed under local, regional, or general anesthesia, depending on the complexity of the procedure and the patient’s preference. Diagnostic hysteroscopy often uses local anesthesia, while operative hysteroscopy may require general anesthesia.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 24 to 48 hours after the procedure to allow for initial recovery and to monitor for any potential complications, such as cramping or light bleeding.Pre-procedure Preparation
Preparation for hysteroscopy involves following specific guidelines from the healthcare provider, which may include fasting before the procedure, adjusting medications, and undergoing pre-operative tests like blood work. International patients should ensure they have all necessary documentation and medical records for the procedure.Procedure Duration
The hysteroscopy procedure typically lasts between 15 to 45 minutes, depending on whether it is diagnostic or operative. During the procedure, the surgeon inserts a thin, lighted tube (hysteroscope) through the cervix into the uterus to examine the uterine lining or perform surgical interventions.Recovery Time
Recovery from hysteroscopy is usually quick, with most patients able to resume light activities the next day. Full recovery typically occurs within a few days. Patients may experience mild cramping or spotting after the procedure, which should subside within a short period.Estimated Cost
The cost of hysteroscopy can vary depending on the purpose of the procedure, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and medications.Post-procedure Care
Post-operative care for hysteroscopy includes managing any mild discomfort, preventing infection, and monitoring for signs of complications. Patients should follow their healthcare provider’s instructions, which may include avoiding sexual intercourse, using tampons, or engaging in strenuous activities for a short period after the procedure. Follow-up appointments may be necessary to discuss findings or results from the procedure. Any signs of complications, such as heavy bleeding, severe pain, or fever, should be reported to the healthcare provider immediately.
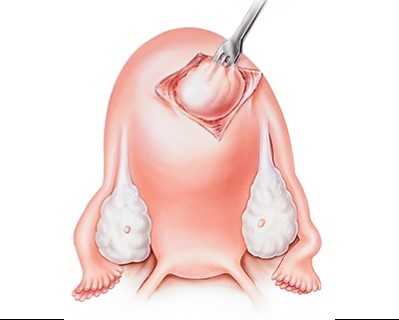
Myomectomy
- Purpose: Removes fibroids from the uterus while preserving fertility.
- Procedure: Fibroids are surgically removed through an abdominal incision, laparoscopically, or hysteroscopically.
-
Note: The information provided here applies to standard Myomectomy procedures under typical conditions. However, specifics may vary based on individual factors, such as the size and location of fibroids, the patient’s overall health, and any complications that might arise during or after the procedure. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Myomectomy can be performed as either an inpatient or outpatient procedure, depending on the size, number, and location of the fibroids, as well as the surgical approach used.Hospital Stay Duration
For more extensive myomectomies, particularly those performed through open surgery, patients may need to stay in the hospital for 1 to 3 days. Minimally invasive myomectomies, such as laparoscopic or hysteroscopic procedures, often allow for same-day discharge or a short overnight stay.Type of Anesthesia
The procedure is typically performed under general anesthesia, ensuring the patient is fully unconscious during the surgery. In some cases, regional anesthesia may be used, particularly for less invasive procedures.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 2 to 4 weeks after the procedure, depending on the surgical approach, to allow for proper healing and to monitor for any potential complications, such as bleeding or infection.Pre-procedure Preparation
Preparation for myomectomy involves following specific instructions from the healthcare provider, such as fasting before surgery, adjusting medications, and undergoing pre-operative tests like blood work and imaging. International patients should ensure they have all necessary documentation and medical records for the procedure.Procedure Duration
The duration of the myomectomy procedure varies depending on the number, size, and location of the fibroids, as well as the surgical technique used. The surgery can take anywhere from 1 to 3 hours.Recovery Time
Recovery time after myomectomy depends on the surgical approach. For open surgery, recovery may take 4 to 6 weeks, while minimally invasive procedures typically allow for a quicker recovery, often within 2 to 4 weeks. Patients are usually advised to avoid heavy lifting and strenuous activities during the recovery period.Estimated Cost
The cost of myomectomy can vary depending on the complexity of the procedure, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and medications.Post-procedure Care
Post-operative care for myomectomy includes managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions for wound care, activity restrictions, and gradually returning to normal activities. Regular follow-up appointments are important to monitor recovery and assess the surgical site. Any signs of complications, such as increased pain, heavy bleeding, or fever, should be reported to the healthcare provider immediately.
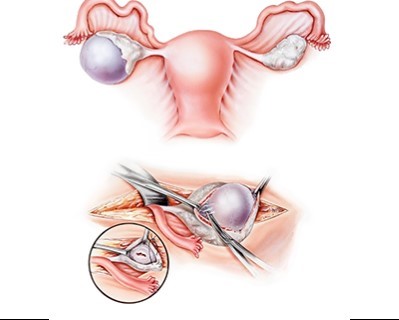
Ovarian Cystectomy
- Purpose: Removes cysts from the ovaries to alleviate pain and prevent complications.
- Procedure: Cysts are surgically removed through an abdominal incision or laparoscopically.
-
Note: The information provided here applies to standard Ovarian Cystectomy procedures under typical conditions. However, specifics may vary based on individual factors, such as the size and type of the ovarian cyst, the patient’s overall health, and any complications that might arise during or after the procedure. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Ovarian cystectomy can be performed as either an inpatient or outpatient procedure, depending on the size and complexity of the cyst, as well as the surgical approach used.Hospital Stay Duration
For minimally invasive procedures, such as laparoscopic ovarian cystectomy, patients are often discharged the same day or after a short overnight stay. In cases of larger or more complex cysts requiring open surgery, a hospital stay of 1 to 2 days may be necessary.Type of Anesthesia
The procedure is typically performed under general anesthesia, ensuring the patient is fully unconscious during the surgery. In some cases, regional anesthesia may be used, particularly for laparoscopic procedures.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 1 to 2 weeks after the procedure to allow for proper healing and to monitor for any potential complications, such as infection or bleeding.Pre-procedure Preparation
Preparation for ovarian cystectomy involves following specific instructions from the healthcare provider, such as fasting before surgery, adjusting medications, and undergoing pre-operative tests like blood work and imaging. International patients should ensure they have all necessary documentation and medical records for the procedure.Procedure Duration
The ovarian cystectomy procedure typically lasts between 1 to 2 hours, depending on the size and complexity of the cyst. The surgeon may use a laparoscopic approach for smaller cysts or open surgery for larger or more complex cases.Recovery Time
Recovery from ovarian cystectomy varies depending on the surgical approach. Patients undergoing laparoscopic surgery may resume light activities within a few days, with full recovery in 2 to 4 weeks. Open surgery may require a longer recovery period of 4 to 6 weeks. Patients should avoid heavy lifting and strenuous activities during recovery.Estimated Cost
The cost of ovarian cystectomy can vary depending on the complexity of the procedure, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and medications.Post-procedure Care
Post-operative care for ovarian cystectomy includes managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions for wound care, activity restrictions, and gradually returning to normal activities. Regular follow-up appointments are important to monitor recovery and assess the surgical site. Any signs of complications, such as increased pain, heavy bleeding, or fever, should be reported to the healthcare provider immediately.
Tubal Ligation
- Purpose: Provides permanent contraception by blocking or sealing the fallopian tubes.
- Procedure: The fallopian tubes are cut, tied, or sealed through laparoscopic or open surgery.
-
Note: The information provided here applies to standard Tubal Ligation procedures under typical conditions. However, specifics may vary based on individual factors, such as the patient’s overall health, the method used for the procedure, and any complications that might arise during or after surgery. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Tubal ligation is typically performed as an outpatient procedure, allowing most patients to return home the same day after a brief recovery period.Hospital Stay Duration
Patients undergoing tubal ligation generally do not require an overnight hospital stay. They are usually discharged a few hours after the procedure, once they have recovered from anesthesia and are stable.Type of Anesthesia
The procedure is usually performed under general anesthesia, ensuring the patient is fully unconscious and pain-free during surgery. In some cases, regional anesthesia may be used, particularly for laparoscopic procedures.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 24 to 48 hours after the procedure to allow for initial recovery and to monitor for any potential complications, such as pain or discomfort at the incision sites.Pre-procedure Preparation
Preparation for tubal ligation involves following specific guidelines from the healthcare provider, such as fasting before surgery, adjusting medications, and undergoing pre-operative tests like blood work. International patients should ensure they have all necessary documentation and medical records for the procedure.Procedure Duration
The tubal ligation procedure typically lasts between 30 minutes to 1 hour. The surgeon either ties, clips, or seals the fallopian tubes to prevent eggs from reaching the uterus, which permanently prevents pregnancy.Recovery Time
Recovery from tubal ligation is generally quick, with most patients able to resume light activities within a few days. Full recovery usually takes about 1 to 2 weeks. Patients should avoid heavy lifting and strenuous activities during the recovery period.Estimated Cost
The cost of tubal ligation can vary depending on the method used, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and medications.Post-procedure Care
Post-operative care for tubal ligation includes managing pain, preventing infection, and ensuring proper healing. Patients may experience some cramping or discomfort at the incision sites, which should subside within a few days. Follow-up appointments are important to monitor recovery and address any concerns. Patients should report any signs of complications, such as severe pain, heavy bleeding, or fever, to their healthcare provider immediately.Legal and Ethical Considerations
Patients considering tubal ligation, particularly in a different country, should be fully informed about the legal regulations surrounding sterilization procedures. Laws regarding consent, age restrictions, and the reversal of tubal ligation can vary between countries. It’s vital to choose a clinic that adheres to ethical standards and provides clear information on the procedure and post-operative care.

Colposcopy
- Purpose: Examines the cervix, vagina, and vulva for signs of disease.
- Procedure: A colposcope is used to magnify and inspect the tissues, and biopsies may be taken.
-
Note: The information provided here applies to standard Colposcopy procedures under typical conditions. However, specifics may vary based on individual factors, such as the patient’s overall health, the findings during the procedure, and any complications that might arise during or after the examination. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Colposcopy is typically performed as an outpatient procedure, allowing most patients to return home the same day shortly after the examination is completed.Hospital Stay Duration
Patients undergoing colposcopy do not require a hospital stay. The procedure is performed in a clinic or outpatient setting, and patients are usually discharged immediately after the procedure.Type of Anesthesia
Colposcopy is usually performed without anesthesia, as it is a minimally invasive procedure. However, if a biopsy is needed, a local anesthetic may be applied to minimize discomfort.Travel After Procedure
Patients are generally able to travel immediately after the procedure, though it’s advisable to avoid strenuous activities for the rest of the day, especially if a biopsy was taken.Pre-procedure Preparation
Preparation for colposcopy may involve avoiding vaginal medications, douching, or sexual intercourse for 24 to 48 hours before the procedure. Patients should follow their healthcare provider’s specific instructions. It’s important to inform the provider of any medications being taken or any potential pregnancy.Procedure Duration
The colposcopy procedure typically lasts between 10 to 20 minutes. During the procedure, the healthcare provider uses a colposcope—a special magnifying instrument—to closely examine the cervix, vagina, and vulva for abnormal areas that may require a biopsy.Recovery Time
Recovery from colposcopy is immediate, though patients who have had a biopsy may experience mild cramping or light spotting for a few days. Most patients can resume normal activities the same day, with the exception of any strenuous physical activity if a biopsy was performed.Estimated Cost
The cost of colposcopy can vary depending on whether a biopsy is needed, the healthcare provider's expertise, and geographic location. Patients should consult their healthcare provider or clinic for detailed cost information, including any additional fees for biopsies or follow-up care.Post-procedure Care
Post-procedure care after colposcopy includes managing any mild discomfort and monitoring for signs of complications. If a biopsy was taken, patients should avoid tampons, douching, and sexual intercourse for a few days to allow the cervix to heal. Follow-up appointments may be necessary to discuss biopsy results. Any signs of complications, such as heavy bleeding, severe pain, or unusual discharge, should be reported to the healthcare provider immediately.
_20240719141710702029__0.webp)
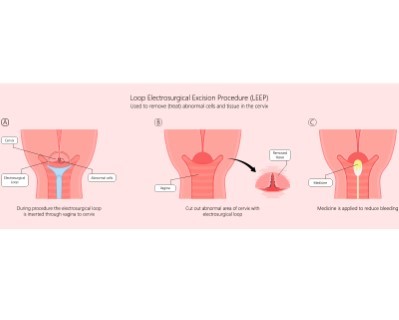
LEEP (Loop Electrosurgical Excision Procedure)
- Purpose: Removes abnormal cervical tissue to prevent cervical cancer.
- Procedure: A thin wire loop heated by electric current is used to excise abnormal tissue.
-
Note: The information provided here applies to standard LEEP procedures under typical conditions. However, specifics may vary based on individual factors, such as the patient’s overall health, the extent of the abnormal tissue, and any complications that might arise during or after the procedure. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
LEEP is typically performed as an outpatient procedure, allowing most patients to return home the same day after the procedure is completed.Hospital Stay Duration
Patients undergoing LEEP generally do not require a hospital stay. The procedure is performed in a clinic or outpatient setting, and patients are usually discharged shortly after the procedure.Type of Anesthesia
LEEP is usually performed under local anesthesia to numb the cervix, making the procedure more comfortable. General anesthesia is rarely needed unless the patient requires a more extensive procedure.Travel After Procedure
Patients are generally able to travel shortly after the procedure, though it is advisable to avoid strenuous activities for the rest of the day. Long-distance travel should be avoided for at least 24 to 48 hours to monitor for any potential complications, such as bleeding or cramping.Pre-procedure Preparation
Preparation for LEEP involves following specific instructions from the healthcare provider, which may include avoiding vaginal medications, douching, or sexual intercourse for 24 to 48 hours before the procedure. Patients should also inform their provider of any medications they are taking or any potential pregnancy.Procedure Duration
The LEEP procedure typically lasts about 10 to 20 minutes. During the procedure, a thin wire loop heated by electric current is used to remove abnormal tissue from the cervix.Recovery Time
Recovery from LEEP is generally quick, with most patients able to resume normal activities within a day or two. Patients may experience mild cramping, light bleeding, or discharge for a few days to a couple of weeks after the procedure. It is important to avoid heavy lifting, strenuous activities, and sexual intercourse for a few weeks to allow the cervix to heal properly.Estimated Cost
The cost of LEEP can vary depending on the healthcare provider's expertise, the complexity of the procedure, and geographic location. Patients should consult their healthcare provider or clinic for detailed cost information, including any additional fees for follow-up care and pathology services.Post-procedure Care
Post-procedure care after LEEP includes managing any discomfort, preventing infection, and monitoring for signs of complications. Patients should follow their healthcare provider’s instructions, which may include avoiding tampons, douching, and sexual intercourse for a few weeks. Follow-up appointments are important to ensure proper healing and to review the pathology results. Any signs of complications, such as heavy bleeding, severe pain, or fever, should be reported to the healthcare provider immediately.
Pelvic Floor Repair Surgery
- Purpose: Treats pelvic organ prolapse and incontinence.
- Procedure: The pelvic floor is repaired through various surgical techniques to support the organs.
-
Note: The information provided here applies to standard Pelvic Floor Repair Surgery procedures under typical conditions. However, specifics may vary based on individual factors, such as the severity of the pelvic floor disorder, the patient’s overall health, and any complications that might arise during or after surgery. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Pelvic floor repair surgery is typically performed as an inpatient procedure, requiring a hospital stay for monitoring and initial recovery.Hospital Stay Duration
Patients undergoing pelvic floor repair surgery usually stay in the hospital for 1 to 3 days, depending on the complexity of the surgery and the patient’s recovery progress. This allows healthcare providers to manage pain, monitor for complications, and begin early rehabilitation.Type of Anesthesia
The procedure is generally performed under general anesthesia, ensuring the patient is fully unconscious and comfortable during surgery. In some cases, regional anesthesia may be used.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 2 to 4 weeks after the procedure to allow for proper healing and to monitor for any potential complications, such as infection or pelvic pain.Pre-procedure Preparation
Preparation for pelvic floor repair surgery involves following specific instructions from the healthcare provider, such as fasting before surgery, adjusting medications, and undergoing pre-operative tests like blood work and imaging. Patients should ensure they have all necessary documentation and medical records if traveling internationally for the procedure.Procedure Duration
The duration of pelvic floor repair surgery varies depending on the extent of the repair needed, but it typically lasts between 2 to 4 hours. The surgery may involve repairing or reinforcing the pelvic floor muscles and tissues to correct conditions such as pelvic organ prolapse.Recovery Time
Recovery from pelvic floor repair surgery can take several weeks. Most patients can resume light activities within 2 to 4 weeks, but full recovery may take up to 6 to 8 weeks or longer. Patients should avoid heavy lifting, strenuous activities, and sexual intercourse during the recovery period, as advised by their healthcare provider.Estimated Cost
The cost of pelvic floor repair surgery can vary based on the complexity of the procedure, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and rehabilitation.Post-procedure Care
Post-operative care for pelvic floor repair surgery includes managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions for wound care, activity restrictions, and gradually returning to normal activities. Physical therapy may be recommended to strengthen the pelvic floor muscles. Regular follow-up appointments are important to monitor recovery and address any concerns. Any signs of complications, such as increased pain, heavy bleeding, or fever, should be reported to the healthcare provider immediately.
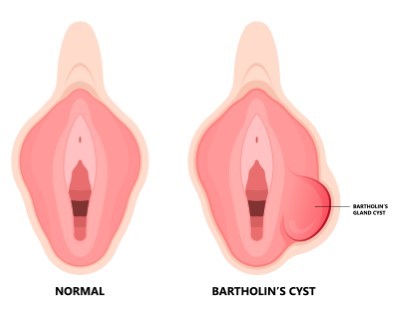
Bartholin Cyst Removal
- Purpose: Removes cysts or abscesses from the Bartholin glands to relieve pain and prevent infection.
- Procedure: The cyst or abscess is surgically drained or removed.
-
Note: The information provided here applies to standard Bartholin Cyst Removal procedures under typical conditions. However, specifics may vary based on individual factors, such as the size of the cyst, the patient’s overall health, and any complications that might arise during or after the procedure. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Bartholin cyst removal is typically performed as an outpatient procedure, allowing most patients to return home the same day after the procedure is completed.Hospital Stay Duration
Patients undergoing Bartholin cyst removal generally do not require a hospital stay. The procedure is performed in a clinic or outpatient setting, and patients are usually discharged shortly after the procedure.Type of Anesthesia
Bartholin cyst removal is usually performed under local anesthesia to numb the area, making the procedure more comfortable. In some cases, sedation or general anesthesia may be used, depending on the patient’s preference and the complexity of the procedure.Travel After Procedure
Patients are generally able to travel shortly after the procedure, though it is advisable to avoid strenuous activities for the rest of the day. Long-distance travel should be avoided for at least 24 to 48 hours to monitor for any potential complications, such as infection or discomfort.Pre-procedure Preparation
Preparation for Bartholin cyst removal involves following specific instructions from the healthcare provider, which may include avoiding certain medications and fasting if sedation or general anesthesia is planned. Patients should inform their provider of any medications they are taking or any potential allergies.Procedure Duration
The Bartholin cyst removal procedure typically lasts about 30 minutes to 1 hour. During the procedure, the surgeon drains the cyst and may remove the gland if necessary to prevent recurrence.Recovery Time
Recovery from Bartholin cyst removal is generally quick, with most patients able to resume normal activities within a few days. Patients may experience mild discomfort, swelling, or light bleeding for a few days after the procedure. It is important to keep the area clean and avoid sexual intercourse for a few weeks to allow for proper healing.Estimated Cost
The cost of Bartholin cyst removal can vary depending on the healthcare provider's expertise, the complexity of the procedure, and geographic location. Patients should consult their healthcare provider or clinic for detailed cost information, including any additional fees for follow-up care and pathology services if the cyst is sent for testing.Post-procedure Care
Post-procedure care after Bartholin cyst removal includes managing any discomfort, preventing infection, and monitoring for signs of complications. Patients should follow their healthcare provider’s instructions, which may include soaking the area in warm water (sitz baths) to promote healing. Any signs of complications, such as increased pain, heavy bleeding, or fever, should be reported to the healthcare provider immediately.
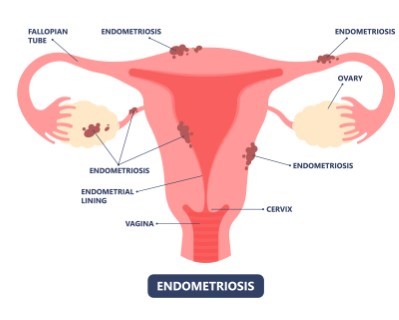
Endometriosis Surgery
- Purpose: Removes or destroys endometrial tissue growing outside the uterus to relieve pain and improve fertility.
- Procedure: Endometrial implants are excised or ablated through laparoscopic surgery.
-
Note: The information provided here applies to standard Endometriosis Surgery procedures under typical conditions. However, specifics may vary based on individual factors, such as the extent of the endometriosis, the patient’s overall health, and any complications that might arise during or after surgery. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Endometriosis surgery can be performed as either an inpatient or outpatient procedure, depending on the extent of the disease and the surgical approach used. Minimally invasive laparoscopic surgery is often performed on an outpatient basis, while more extensive surgery may require an inpatient stay.Hospital Stay Duration
For minimally invasive procedures, patients may be discharged the same day or after a short overnight stay. More extensive surgery may require a hospital stay of 1 to 3 days for monitoring and initial recovery.Type of Anesthesia
Endometriosis surgery is typically performed under general anesthesia, ensuring the patient is fully unconscious and comfortable during the procedure.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 2 to 4 weeks after surgery to allow for proper healing and to monitor for any potential complications, such as infection or post-operative pain.Pre-procedure Preparation
Preparation for endometriosis surgery involves following specific instructions from the healthcare provider, such as fasting before surgery, adjusting medications, and undergoing pre-operative tests like blood work and imaging. Patients traveling internationally should ensure they have all necessary documentation and medical records.Procedure Duration
The duration of endometriosis surgery varies depending on the extent of the disease and the surgical technique used, but it typically lasts between 1 to 3 hours. The surgeon may remove or destroy endometrial tissue using a laparoscope or perform more extensive surgery to remove adhesions and restore normal anatomy.Recovery Time
Recovery from endometriosis surgery varies depending on the procedure's complexity. For laparoscopic surgery, most patients can resume light activities within 1 to 2 weeks, with full recovery taking 4 to 6 weeks. More extensive surgery may require a longer recovery period. Patients should avoid heavy lifting and strenuous activities during recovery.Estimated Cost
The cost of endometriosis surgery can vary depending on the complexity of the procedure, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and medications.Post-procedure Care
Post-operative care for endometriosis surgery includes managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions for wound care, activity restrictions, and gradually returning to normal activities. Follow-up appointments are essential to monitor recovery and address any concerns. Any signs of complications, such as increased pain, heavy bleeding, or fever, should be reported to the healthcare provider immediately.

Laparoscopic Oophorectomy
- Purpose: Removes one or both ovaries to treat conditions such as ovarian cancer or severe endometriosis.
- Procedure: The ovaries are surgically removed using laparoscopic techniques.
-
Note: The information provided here applies to standard Laparoscopic Oophorectomy procedures under typical conditions. However, specifics may vary based on individual factors, such as the patient’s overall health, the reason for the oophorectomy, and any complications that might arise during or after surgery. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Laparoscopic oophorectomy is typically performed as an outpatient procedure, allowing most patients to return home the same day after the surgery is completed. However, depending on the complexity of the procedure, some patients may require an overnight hospital stay.Hospital Stay Duration
Patients undergoing laparoscopic oophorectomy generally do not require an extended hospital stay. Most are discharged a few hours after surgery, once they have recovered from anesthesia and are stable. In cases of more extensive surgery, a 1-day hospital stay may be recommended.Type of Anesthesia
The procedure is performed under general anesthesia, ensuring the patient is fully unconscious and comfortable during the surgery.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 1 to 2 weeks after the procedure to allow for proper healing and to monitor for any potential complications, such as bleeding or infection.Pre-procedure Preparation
Preparation for laparoscopic oophorectomy involves following specific guidelines from the healthcare provider, such as fasting before surgery, adjusting medications, and undergoing pre-operative tests like blood work and imaging. International patients should ensure they have all necessary documentation and medical records.Procedure Duration
The laparoscopic oophorectomy procedure typically lasts between 1 to 2 hours, depending on the reason for the surgery and the complexity of the case. During the procedure, the surgeon removes one or both ovaries using small incisions and specialized instruments, often employing a laparoscope for visual guidance.Recovery Time
Recovery from laparoscopic oophorectomy is generally quicker than open surgery. Most patients can resume light activities within 1 to 2 weeks, with full recovery taking about 4 to 6 weeks. Patients should avoid heavy lifting and strenuous activities during the recovery period.Estimated Cost
The cost of laparoscopic oophorectomy can vary depending on the complexity of the procedure, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and medications.Post-procedure Care
Post-operative care for laparoscopic oophorectomy includes managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions for wound care, activity restrictions, and gradually returning to normal activities. Regular follow-up appointments are important to monitor recovery and address any concerns. Any signs of complications, such as increased pain, heavy bleeding, or fever, should be reported to the healthcare provider immediately.

Labiaplasty
- Purpose: Reshapes or reduces the size of the labia for cosmetic or medical reasons.
- Procedure: Excess tissue is removed or reshaped through surgical techniques.
-
Note: The information provided here applies to standard Labiaplasty procedures under typical conditions. However, specifics may vary based on individual factors, such as the patient’s overall health, the extent of the surgery, and any complications that might arise during or after the procedure. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Labiaplasty is typically performed as an outpatient procedure, allowing most patients to return home the same day after the surgery is completed.Hospital Stay Duration
Patients undergoing labiaplasty generally do not require a hospital stay. They are usually discharged a few hours after the procedure, once they have recovered from anesthesia and are stable.Type of Anesthesia
Labiaplasty is commonly performed under local anesthesia with sedation to keep the patient comfortable. In some cases, general anesthesia may be used, depending on the patient’s preference and the surgeon’s recommendation.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 1 to 2 weeks after the procedure to allow for proper healing and to monitor for any potential complications, such as swelling or discomfort.Pre-procedure Preparation
Preparation for labiaplasty involves following specific instructions from the healthcare provider, such as fasting before surgery, adjusting medications, and avoiding certain activities or products. Patients should ensure they have all necessary documentation and medical records if traveling internationally for the procedure.Procedure Duration
The labiaplasty procedure typically lasts between 1 to 2 hours, depending on the extent of the surgery. The surgeon carefully trims or reshapes the labia minora and/or labia majora to achieve the desired results.Recovery Time
Recovery from labiaplasty is generally quick, with most patients able to resume light activities within a few days. Full recovery typically takes 4 to 6 weeks. During this time, patients should avoid sexual activity, strenuous exercise, and wearing tight clothing to ensure proper healing.Estimated Cost
The cost of labiaplasty can vary depending on the complexity of the procedure, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and medications.Post-procedure Care
Post-operative care for labiaplasty includes managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions for wound care, activity restrictions, and gradually returning to normal activities. Ice packs and prescribed pain medications can help manage swelling and discomfort. Follow-up appointments are important to monitor recovery and address any concerns. Any signs of complications, such as increased pain, heavy bleeding, or signs of infection, should be reported to the healthcare provider immediately.

Hysteroscopic Myomectomy
- Purpose: Removes fibroids from the uterus using a hysteroscope to improve symptoms and fertility.
- Procedure: A hysteroscope is inserted through the cervix to remove fibroids from the uterine cavity.
-
Note: The information provided here applies to standard Hysteroscopic Myomectomy procedures under typical conditions. However, specifics may vary based on individual factors, such as the size and location of the fibroids, the patient’s overall health, and any complications that might arise during or after the procedure. Patients seeking this procedure through health tourism should also consider local regulations and the importance of choosing a reputable clinic that adheres to international standards.
Inpatient/Outpatient
Hysteroscopic myomectomy is typically performed as an outpatient procedure, allowing most patients to return home the same day after the surgery is completed.Hospital Stay Duration
Patients undergoing hysteroscopic myomectomy generally do not require a hospital stay. They are usually discharged a few hours after the procedure, once they have recovered from anesthesia and are stable.Type of Anesthesia
The procedure is commonly performed under general anesthesia to ensure the patient is fully unconscious and comfortable. In some cases, regional anesthesia may be used, depending on the patient’s condition and the surgeon’s preference.Travel After Procedure
Patients are generally advised to avoid long-distance travel for at least 1 to 2 weeks after the procedure to allow for proper healing and to monitor for any potential complications, such as bleeding or discomfort.Pre-procedure Preparation
Preparation for hysteroscopic myomectomy involves following specific guidelines from the healthcare provider, such as fasting before surgery, adjusting medications, and undergoing pre-operative tests like blood work and imaging. Patients traveling internationally should ensure they have all necessary documentation and medical records.Procedure Duration
The hysteroscopic myomectomy procedure typically lasts between 1 to 2 hours, depending on the size and number of fibroids being removed. The surgeon uses a hysteroscope (a thin, lighted tube) inserted through the cervix to remove the fibroids from the uterus.Recovery Time
Recovery from hysteroscopic myomectomy is generally quick, with most patients able to resume light activities within a few days. Full recovery typically takes about 1 to 2 weeks. Patients should avoid heavy lifting, strenuous activities, and sexual intercourse during the recovery period to ensure proper healing.Estimated Cost
The cost of hysteroscopic myomectomy can vary depending on the complexity of the procedure, the surgeon's expertise, and geographic location. Patients should consult their healthcare provider or surgical center for detailed cost information, including any additional fees for follow-up care and medications.Post-procedure Care
Post-operative care for hysteroscopic myomectomy includes managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions for wound care, activity restrictions, and gradually returning to normal activities. Mild cramping, spotting, or discharge is common after the procedure, but any signs of complications, such as heavy bleeding, severe pain, or fever, should be reported to the healthcare provider immediately.
