Eear nose throat Treatments
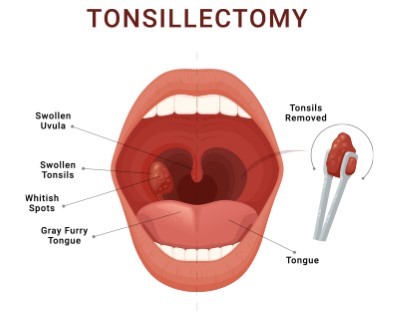
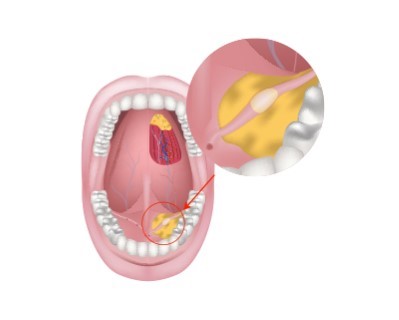
Tonsillectomy
- Purpose: Removes the tonsils to treat recurrent throat infections and sleep apnea.
- Procedure: The tonsils are surgically removed through the mouth.
-
Note: The information provided here applies to routine tonsillectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of recurrent infections, the patient’s age, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Tonsillectomy is typically performed as an outpatient procedure, especially in older children and adults. This means that most patients can return home the same day after a short observation period. In some cases, particularly for young children or patients with other health issues, an overnight stay may be required for closer monitoring.Hospital Stay Duration
Patients undergoing tonsillectomy generally do not require an overnight hospital stay unless there are complications or other medical conditions that necessitate extended monitoring. The surgery itself usually takes about 30 to 60 minutes, and patients are typically discharged within a few hours after the procedure, once they are fully awake and able to swallow liquids.Type of Anesthesia
Tonsillectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. General anesthesia is necessary to keep the patient comfortable and still, allowing the surgical team to safely remove the tonsils.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least a week after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as bleeding. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for tonsillectomy typically involves following specific guidelines provided by the healthcare provider. Patients (or their caregivers) may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery.Procedure Duration
The tonsillectomy procedure typically takes about 30 to 60 minutes. During the surgery, the tonsils are removed through the mouth using surgical instruments. The procedure may also involve cauterization to reduce bleeding. In some cases, the adenoids may also be removed, especially if they are enlarged or causing breathing issues.Recovery Time
Recovery from tonsillectomy can take 1 to 2 weeks. Most patients experience throat pain, difficulty swallowing, and mild ear pain during the recovery period. A soft or liquid diet is usually recommended to avoid irritating the surgical site. It is important to stay hydrated and follow pain management instructions provided by the healthcare provider. Patients should avoid strenuous activities and contact sports for at least 2 weeks to reduce the risk of bleeding.Estimated Cost
The cost of tonsillectomy can vary depending on the hospital, geographic location, and whether the procedure is performed as part of a broader treatment plan. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for tonsillectomy involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow dietary recommendations, which typically include soft foods, cold liquids, and avoiding acidic or spicy foods. Monitoring for signs of complications, such as bleeding, dehydration, or infection, is essential. Follow-up appointments may be scheduled to check the healing progress. In the case of any severe pain, fever, or significant bleeding, patients should seek immediate medical attention.
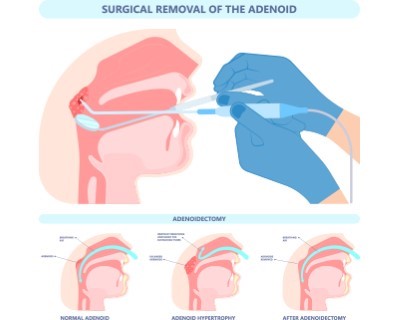
Adenoidectomy
- Purpose: Removes the adenoids to treat breathing problems, chronic infections, and earaches.
- Procedure: The adenoids are surgically removed through the mouth.
-
Note: The information provided here applies to routine adenoidectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of recurrent infections, breathing difficulties, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Adenoidectomy is typically performed as an outpatient procedure, especially in older children and adults. This means that most patients can return home the same day after a short observation period. In some cases, particularly for young children or patients with other health issues, an overnight stay may be required for closer monitoring.Hospital Stay Duration
Patients undergoing adenoidectomy generally do not require an overnight hospital stay unless there are complications or other medical conditions that necessitate extended monitoring. The surgery itself usually takes about 20 to 30 minutes, and patients are typically discharged within a few hours after the procedure, once they are fully awake and able to swallow liquids.Type of Anesthesia
Adenoidectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. General anesthesia is necessary to keep the patient comfortable and still, allowing the surgical team to safely remove the adenoids.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least a week after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as bleeding. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for adenoidectomy typically involves following specific guidelines provided by the healthcare provider. Patients (or their caregivers) may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery.Procedure Duration
The adenoidectomy procedure typically takes about 20 to 30 minutes. During the surgery, the adenoids are removed through the mouth using surgical instruments. The procedure may also involve cauterization to reduce bleeding. In some cases, a tonsillectomy may be performed simultaneously, especially if the patient has recurrent throat infections or obstructive sleep apnea.Recovery Time
Recovery from adenoidectomy is generally quicker than from tonsillectomy, with most patients recovering within 1 to 2 weeks. Most patients experience mild throat discomfort, nasal congestion, and ear pain during the recovery period. A soft or liquid diet is usually recommended to avoid irritating the surgical site. It is important to stay hydrated and follow pain management instructions provided by the healthcare provider. Patients should avoid strenuous activities and contact sports for at least 1 week to reduce the risk of bleeding.Estimated Cost
The cost of adenoidectomy can vary depending on the hospital, geographic location, and whether the procedure is performed as part of a broader treatment plan. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for adenoidectomy involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow dietary recommendations, which typically include soft foods, cold liquids, and avoiding acidic or spicy foods. Monitoring for signs of complications, such as bleeding, dehydration, or infection, is essential. Follow-up appointments may be scheduled to check the healing progress. In the case of any severe pain, fever, or significant bleeding, patients should seek immediate medical attention.
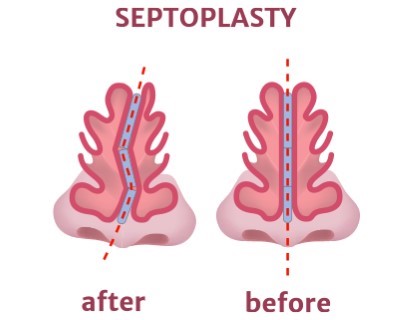
Septoplasty
- Purpose: Corrects a deviated septum to improve breathing and reduce nasal congestion.
- Procedure: The nasal septum is surgically straightened.
-
Note: The information provided here applies to routine septoplasty procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the severity of the deviated septum, patient tolerance, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions (e.g., turbinate reduction) can also influence the surgery and recovery process.
Inpatient/Outpatient
Septoplasty is typically performed as an outpatient procedure. This means that most patients can return home the same day after a short observation period. In some cases, particularly if additional procedures are performed or if there are concerns about post-operative complications, an overnight stay may be required for closer monitoring.Hospital Stay Duration
Patients undergoing septoplasty generally do not require an overnight hospital stay unless there are complications or other medical conditions that necessitate extended monitoring. The surgery itself usually takes about 30 to 90 minutes, depending on the complexity of the septal deviation and whether additional procedures are performed. Patients are typically discharged within a few hours after the procedure, once they are fully awake and stable.Type of Anesthesia
Septoplasty is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. In some cases, local anesthesia with sedation may be used, allowing the patient to remain relaxed and comfortable while still conscious. The choice of anesthesia depends on the patient’s preference and the surgeon’s recommendation.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as bleeding or swelling. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for septoplasty typically involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery. Smoking should be avoided to enhance healing and reduce the risk of complications.Procedure Duration
The septoplasty procedure typically takes about 30 to 90 minutes. During the surgery, the surgeon makes an incision inside the nostril to access the nasal septum. The deviated portions of the septum are then repositioned or removed to improve airflow. If necessary, other structures within the nose, such as the turbinates, may also be adjusted to further enhance breathing. The incision is usually closed with dissolvable stitches, and splints or soft packing may be placed in the nostrils to support the septum as it heals.Recovery Time
Recovery from septoplasty can take 1 to 2 weeks. Most patients experience nasal congestion, mild pain, and swelling during the initial recovery period. It is common to have some nasal discharge or mild bleeding for a few days after the procedure. Patients are usually advised to avoid strenuous activities, heavy lifting, and bending over for at least 2 weeks to minimize the risk of bleeding. Sleeping with the head elevated and avoiding blowing the nose can help reduce swelling and discomfort. Full recovery, including the resolution of swelling and improvement in breathing, can take several weeks to a few months.Estimated Cost
The cost of septoplasty can vary depending on the hospital, geographic location, and whether the procedure is performed as part of a broader treatment plan (e.g., combined with rhinoplasty or turbinate reduction). For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for septoplasty involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the nose after surgery, including cleaning the nostrils gently and using saline sprays to keep the nasal passages moist. Follow-up appointments may be scheduled to check the healing progress, remove splints if placed, and address any concerns. In the case of any severe pain, fever, significant bleeding, or difficulty breathing, patients should seek immediate medical attention.
_20240719140051969332__0.webp)
Functional Endoscopic Sinus Surgery (FESS)
- Purpose: Treats chronic sinusitis and nasal polyps by improving sinus drainage.
- Procedure: A small endoscope is inserted into the nose to remove blockages and improve sinus function.
-
Note: The information provided here applies to routine Functional Endoscopic Sinus Surgery (FESS) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the severity of sinus disease, patient tolerance, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
FESS is typically performed as an outpatient procedure. This means that most patients can return home the same day after a short observation period. In some cases, particularly if extensive sinus surgery is performed or if there are concerns about post-operative complications, an overnight stay may be required for closer monitoring.Hospital Stay Duration
Patients undergoing FESS generally do not require an overnight hospital stay unless there are complications or other medical conditions that necessitate extended monitoring. The surgery itself usually takes about 1 to 3 hours, depending on the complexity of the sinus disease and whether additional procedures are performed. Patients are typically discharged within a few hours after the procedure, once they are fully awake and stable.Type of Anesthesia
FESS is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. In some cases, local anesthesia with sedation may be used, allowing the patient to remain relaxed and comfortable while still conscious. The choice of anesthesia depends on the patient’s preference and the surgeon’s recommendation.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as bleeding or swelling. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for FESS typically involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery. Smoking should be avoided to enhance healing and reduce the risk of complications. Pre-operative imaging studies, such as a CT scan, are often required to plan the surgery.Procedure Duration
The FESS procedure typically takes about 1 to 3 hours. During the surgery, an endoscope is inserted through the nostrils to visualize the sinuses. The surgeon uses specialized instruments to remove blockages, polyps, or damaged tissue to restore normal drainage and function of the sinuses. The goal is to improve airflow, reduce the frequency and severity of sinus infections, and alleviate symptoms such as congestion and facial pain. Depending on the patient’s condition, other procedures, such as septoplasty or turbinate reduction, may be performed simultaneously.Recovery Time
Recovery from FESS can take 1 to 2 weeks. Most patients experience nasal congestion, mild pain, and swelling during the initial recovery period. Some nasal discharge or mild bleeding is common for the first few days after surgery. Patients are usually advised to avoid strenuous activities, heavy lifting, and bending over for at least 2 weeks to minimize the risk of bleeding. Sleeping with the head elevated and using saline sprays can help reduce swelling and discomfort. Full recovery, including the resolution of swelling and improvement in sinus function, can take several weeks to a few months.Estimated Cost
The cost of FESS can vary depending on the hospital, geographic location, and whether the procedure is performed as part of a broader treatment plan. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for FESS involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the nose and sinuses after surgery, including regular saline irrigation to keep the nasal passages clean and moist. Follow-up appointments are essential to monitor healing, remove any packing or splints, and assess the overall success of the surgery. In the case of any severe pain, fever, significant bleeding, or difficulty breathing, patients should seek immediate medical attention.
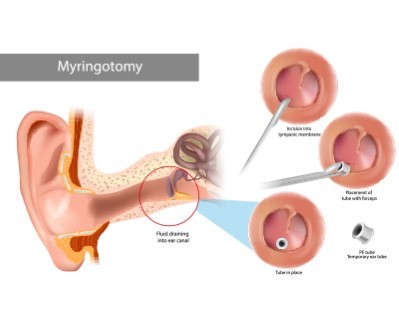
Myringotomy with Tube Insertion
- Purpose: Treats chronic ear infections and fluid buildup by allowing drainage from the middle ear.
- Procedure: A small incision is made in the eardrum, and a tube is inserted to facilitate drainage.
-
Note: The information provided here applies to routine Myringotomy with Tube Insertion procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the severity of ear infections, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Myringotomy with Tube Insertion is typically performed as an outpatient procedure. This means that most patients, including young children, can return home the same day after a short observation period. The procedure is usually conducted in a hospital or surgical center, where patients are monitored to ensure they recover safely from anesthesia.Hospital Stay Duration
Patients undergoing Myringotomy with Tube Insertion generally do not require an overnight hospital stay unless there are complications or other medical conditions that necessitate extended monitoring. The procedure itself is relatively quick, usually taking about 15 to 30 minutes. Patients are typically discharged within a few hours after the procedure, once they are fully awake and stable.Type of Anesthesia
Myringotomy with Tube Insertion is commonly performed under general anesthesia in young children to keep them comfortable and still during the procedure. For older children and adults, local anesthesia with or without sedation may be used. The choice of anesthesia depends on the patient’s age, comfort level, and the surgeon’s recommendation.Travel After Procedure
Patients are generally able to travel shortly after the procedure, though it is advisable to rest for the remainder of the day. Long-distance travel is usually safe within a day or two, but patients should follow specific recommendations from their healthcare provider regarding travel and activity levels.Pre-procedure Preparation
Preparation for Myringotomy with Tube Insertion typically involves following specific guidelines provided by the healthcare provider. For children undergoing general anesthesia, fasting for several hours before the procedure is usually required, typically after midnight the night before. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery.Procedure Duration
The Myringotomy with Tube Insertion procedure typically takes about 15 to 30 minutes. During the procedure, a small incision is made in the eardrum (tympanic membrane) to allow fluid to drain from the middle ear. A tiny tube (tympanostomy tube) is then inserted into the incision to ventilate the ear and prevent further fluid buildup. The tubes usually remain in place for several months to a year, after which they may fall out on their own or be removed by the doctor.Recovery Time
Recovery from Myringotomy with Tube Insertion is generally quick, with most patients able to resume normal activities the following day. Mild discomfort or ear drainage may occur for a few days after the procedure. Patients are usually advised to avoid getting water in the ears during bathing or swimming to prevent infection. The healthcare provider will provide specific aftercare instructions, including how to protect the ears and when to follow up for tube monitoring.Estimated Cost
The cost of Myringotomy with Tube Insertion can vary depending on the hospital, geographic location, and whether the procedure is performed as part of a broader treatment plan for chronic ear infections. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for Myringotomy with Tube Insertion involves monitoring the ears for signs of infection, such as redness, pain, or unusual drainage. Patients may be prescribed antibiotic ear drops to prevent infection after the procedure. It is important to follow the healthcare provider’s instructions on how to care for the ears, including avoiding water exposure and using earplugs as recommended. Regular follow-up appointments are essential to monitor the position of the tubes and to assess the overall success of the procedure. If the tubes fall out prematurely or if any complications arise, additional treatment may be required.

Rhinoplasty
- Purpose: Reshapes the nose to improve appearance or correct structural issues.
- Procedure: Surgical techniques are used to modify the bone and cartilage of the nose.
-
Note: The information provided here applies to elective Rhinoplasty procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the complexity of the surgery, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the extent of the desired changes, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Rhinoplasty is typically performed as an outpatient procedure. This means that most patients can return home the same day after a short observation period. However, in cases of more extensive surgery or if there are concerns about post-operative complications, an overnight stay may be required for closer monitoring.Hospital Stay Duration
Patients undergoing rhinoplasty generally do not require an overnight hospital stay unless the procedure is particularly complex or if there are medical conditions that necessitate extended monitoring. The surgery itself usually takes about 1 to 3 hours, depending on the complexity of the procedure. Patients are typically discharged within a few hours after the procedure, once they are fully awake and stable.Type of Anesthesia
Rhinoplasty is usually performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. In some cases, local anesthesia with sedation may be used, allowing the patient to remain relaxed and comfortable while still conscious. The choice of anesthesia depends on the patient’s preference, the extent of the surgery, and the surgeon’s recommendation.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as bleeding or swelling. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for rhinoplasty typically involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery. Smoking should be avoided to enhance healing and reduce the risk of complications.Procedure Duration
The rhinoplasty procedure typically takes about 1 to 3 hours, depending on the complexity of the surgery. During the procedure, the surgeon reshapes the nose by adjusting the bone, cartilage, and soft tissues to achieve the desired appearance and function. Rhinoplasty can address a variety of issues, including a crooked nose, a hump on the nasal bridge, a drooping nasal tip, or breathing difficulties. Depending on the patient’s needs, the surgery may be performed using an open or closed technique, with incisions made either inside the nostrils or across the columella (the tissue between the nostrils).Recovery Time
Recovery from rhinoplasty can take several weeks. Most patients experience swelling, bruising, and nasal congestion during the initial recovery period. A splint is usually placed on the nose to support the new shape and protect the area during healing. Patients are typically advised to avoid strenuous activities, heavy lifting, and contact sports for at least 4 to 6 weeks to minimize the risk of complications. It is important to sleep with the head elevated and avoid blowing the nose for several weeks after surgery. Full recovery, including the resolution of swelling and the final appearance of the nose, can take up to a year.Estimated Cost
The cost of rhinoplasty can vary widely depending on the surgeon's expertise, the complexity of the procedure, geographic location, and whether the surgery is performed for cosmetic or functional reasons (such as correcting a deviated septum). For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for rhinoplasty involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the nose after surgery, including cleaning the incision sites gently and using cold compresses to reduce swelling. Follow-up appointments are essential to monitor healing, remove stitches and the nasal splint, and assess the overall success of the surgery. In the case of any severe pain, fever, significant bleeding, or difficulty breathing, patients should seek immediate medical attention.

Tympanoplasty
- Purpose: Repairs a perforated eardrum to restore hearing and prevent infections.
- Procedure: The eardrum is surgically reconstructed using graft material.
-
Note: The information provided here applies to routine Tympanoplasty procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the severity of the ear condition, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the surgery, and the need for additional interventions (e.g., ossiculoplasty) can also influence the surgery and recovery process.
Inpatient/Outpatient
Tympanoplasty is typically performed as an outpatient procedure, meaning that most patients can return home the same day after a short observation period. However, in cases where the surgery is more complex or if there are concerns about post-operative complications, an overnight stay may be required for closer monitoring.Hospital Stay Duration
Patients undergoing tympanoplasty generally do not require an overnight hospital stay unless the procedure is particularly complex or if there are medical conditions that necessitate extended monitoring. The surgery itself usually takes about 1 to 2 hours, depending on the complexity of the ear damage and whether additional procedures are performed. Patients are typically discharged within a few hours after the procedure, once they are fully awake and stable.Type of Anesthesia
Tympanoplasty is usually performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. In some cases, local anesthesia with sedation may be used, especially for less extensive procedures. The choice of anesthesia depends on the patient’s preference, the extent of the surgery, and the surgeon’s recommendation.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as bleeding, dizziness, or infection. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for tympanoplasty typically involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery. Smoking should be avoided to enhance healing and reduce the risk of complications.Procedure Duration
The tympanoplasty procedure typically takes about 1 to 2 hours, depending on the complexity of the surgery. During the procedure, the surgeon repairs the eardrum (tympanic membrane) by grafting tissue, often taken from the patient’s own body, such as from the ear itself or from behind the ear. If there is damage to the bones of the middle ear (ossicles), the surgeon may also perform ossiculoplasty to restore hearing function. The goal of tympanoplasty is to close the perforation in the eardrum, prevent recurrent ear infections, and improve hearing.Recovery Time
Recovery from tympanoplasty can take several weeks. Most patients experience mild ear discomfort, temporary hearing loss, and some drainage or bleeding from the ear during the initial recovery period. Patients are typically advised to avoid getting water in the ear, strenuous activities, and any activities that involve changes in ear pressure, such as flying or diving, for several weeks. It is important to avoid blowing the nose forcefully to prevent pressure changes that could disrupt the healing process. Full recovery, including the improvement in hearing, may take several months, depending on the extent of the repair.Estimated Cost
The cost of tympanoplasty can vary depending on the surgeon's expertise, the complexity of the procedure, geographic location, and whether the surgery is performed in conjunction with other procedures, such as ossiculoplasty. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for tympanoplasty involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the ear after surgery, including keeping the ear dry and avoiding any activities that could increase ear pressure. Follow-up appointments are essential to monitor healing, remove any packing or sutures, and assess the overall success of the surgery. In the case of any severe pain, fever, significant bleeding, or dizziness, patients should seek immediate medical attention.
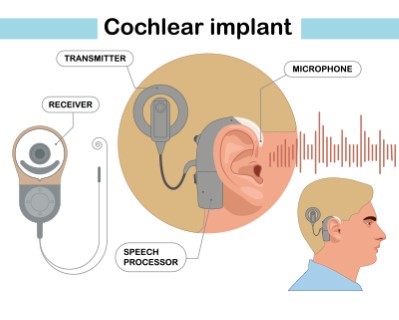
Cochlear Implant Surgery
- Purpose: Provides a sense of sound to individuals with severe hearing loss.
- Procedure: An electronic device is surgically implanted in the ear to stimulate the auditory nerve.
-
Note: The information provided here applies to routine Cochlear Implant Surgery under standard conditions. However, specifics may vary depending on individual patient factors, such as the severity of hearing loss, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the surgery, and the need for additional interventions (e.g., rehabilitation therapy) can also influence the surgery and recovery process.
Inpatient/Outpatient
Cochlear Implant Surgery is typically performed as an inpatient or outpatient procedure. Many patients can return home the same day, but in some cases, particularly if the surgery is more complex or if the patient has other medical conditions, an overnight stay may be required for closer monitoring.Hospital Stay Duration
Patients undergoing Cochlear Implant Surgery generally do not require an extended hospital stay unless there are complications or other medical conditions that necessitate longer monitoring. The surgery itself usually takes about 2 to 4 hours, depending on the complexity of the case. Patients are typically discharged within a few hours after the procedure, once they are fully awake and stable.Type of Anesthesia
Cochlear Implant Surgery is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. This ensures the patient is comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as dizziness or infection. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for Cochlear Implant Surgery typically involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. A comprehensive pre-operative assessment, including hearing tests, imaging studies (such as an MRI or CT scan), and a consultation with an audiologist and surgeon, is conducted to plan the surgery. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery.Procedure Duration
The Cochlear Implant Surgery procedure typically takes about 2 to 4 hours. During the procedure, an incision is made behind the ear, and the surgeon places the internal component of the cochlear implant, which includes a receiver-stimulator and an electrode array that is inserted into the cochlea. The external component, which includes a microphone, speech processor, and transmitter, is fitted a few weeks after surgery once the surgical site has healed. The goal of the procedure is to provide a sense of sound to individuals with severe to profound hearing loss who do not benefit from conventional hearing aids.Recovery Time
Recovery from Cochlear Implant Surgery can take several weeks. Most patients experience mild pain, dizziness, or discomfort around the surgical site during the initial recovery period. It is important to avoid strenuous activities, heavy lifting, and getting the surgical site wet for several weeks. Patients will have a follow-up appointment about 1 to 2 weeks after surgery to assess healing and to remove stitches if necessary. The external components of the cochlear implant are typically activated 2 to 4 weeks after surgery, followed by a series of programming and rehabilitation sessions to optimize the device's performance and to help the patient adjust to hearing through the implant.Estimated Cost
The cost of Cochlear Implant Surgery can vary widely depending on the surgeon's expertise, the complexity of the procedure, geographic location, and whether the surgery is part of a broader treatment plan that includes pre-operative assessments and post-operative rehabilitation. Cochlear implants are often covered by insurance, but out-of-pocket expenses can still be significant. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for Cochlear Implant Surgery involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the surgical site after surgery, including keeping the area clean and dry. Follow-up appointments are essential to monitor healing and to begin the process of activating and programming the cochlear implant. Audiological rehabilitation, which includes learning to interpret the new signals provided by the implant, is a critical part of the post-operative care and is essential for achieving the best possible outcome. In the case of any severe pain, fever, significant swelling, or issues with the implant, patients should seek immediate medical attention.
_20240719140200525144__0.webp)
Uvulopalatopharyngoplasty (UPPP)
- Purpose: Treats obstructive sleep apnea by removing excess tissue from the throat.
- Procedure: The uvula, part of the soft palate, and other tissues are surgically removed to widen the airway.
-
Note: The information provided here applies to routine Uvulopalatopharyngoplasty (UPPP) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the severity of obstructive sleep apnea (OSA) or snoring, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the surgery, and the need for additional interventions (e.g., tonsillectomy or septoplasty) can also influence the surgery and recovery process.
Inpatient/Outpatient
UPPP is typically performed as an inpatient procedure, though some cases may be handled on an outpatient basis, depending on the complexity of the surgery and the patient’s overall health. This surgery involves the removal of excess tissue from the throat to widen the airway, which can help reduce or eliminate snoring and obstructive sleep apnea. Most patients require close monitoring post-surgery, particularly for breathing and airway stability, which may necessitate an overnight stay.Hospital Stay Duration
Patients undergoing UPPP generally require an overnight hospital stay for monitoring, particularly for potential breathing difficulties or complications such as bleeding. The surgery itself usually takes about 1 to 2 hours, depending on the extent of the tissue removal and whether additional procedures are performed. Patients are typically discharged the day after surgery if they are stable and there are no complications.Type of Anesthesia
UPPP is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. This ensures the patient is comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as bleeding or swelling. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for UPPP typically involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery. Smoking should be avoided to enhance healing and reduce the risk of complications. Patients may also need to undergo a sleep study or other evaluations to assess the severity of obstructive sleep apnea and to determine the most appropriate treatment plan.Procedure Duration
The UPPP procedure typically takes about 1 to 2 hours. During the surgery, the surgeon removes excess tissue from the throat, including part of the uvula, soft palate, and possibly the tonsils, to widen the airway. This helps to reduce the obstruction that causes snoring and obstructive sleep apnea. The extent of tissue removal and any additional procedures, such as a tonsillectomy or septoplasty, will depend on the patient’s specific condition.Recovery Time
Recovery from UPPP can take several weeks. Most patients experience significant throat pain, difficulty swallowing, and swelling during the initial recovery period. Pain management is crucial, and patients are usually prescribed pain relievers to help manage discomfort. A soft or liquid diet is typically recommended for the first few weeks to avoid irritating the surgical site. Patients are advised to avoid strenuous activities, heavy lifting, and activities that could increase throat pressure, such as forceful coughing or sneezing, for at least 2 weeks. Full recovery, including the resolution of swelling and improvement in breathing and sleep quality, can take several weeks to a few months.Estimated Cost
The cost of UPPP can vary depending on the surgeon's expertise, the complexity of the procedure, geographic location, and whether the surgery is performed in conjunction with other procedures, such as a tonsillectomy or septoplasty. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for UPPP involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the throat after surgery, including avoiding irritants such as smoking and alcohol. Patients should stay hydrated and follow a soft or liquid diet until swallowing becomes more comfortable. Follow-up appointments are essential to monitor healing, assess the effectiveness of the surgery in reducing snoring and sleep apnea symptoms, and address any complications. In the case of any severe pain, fever, significant bleeding, or difficulty breathing, patients should seek immediate medical attention.

Laryngectomy
- Purpose: Removes the larynx to treat laryngeal cancer.
- Procedure: The larynx is surgically removed, and a stoma (hole) is created in the neck for breathing.
-
Note: The information provided here applies to routine Laryngectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the extent of cancer or other conditions necessitating the surgery, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the surgery, and the need for additional treatments (e.g., radiation therapy) can also influence the surgery and recovery process.
Inpatient/Outpatient
Laryngectomy is typically performed as an inpatient procedure. Given the complexity and seriousness of the surgery, patients will require a hospital stay for close monitoring and to begin the initial phases of recovery and rehabilitation. This surgery involves the removal of the larynx (voice box) and is often necessary for advanced laryngeal cancer or severe trauma to the larynx.Hospital Stay Duration
Patients undergoing laryngectomy generally require a hospital stay of 7 to 14 days, depending on the complexity of the surgery and the patient’s overall condition. The initial days post-surgery are crucial for monitoring the airway, managing pain, and beginning the healing process. Patients will need to stay in the hospital until they are stable, able to manage breathing and feeding with assistance, and ready to continue recovery at home.Type of Anesthesia
Laryngectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. This ensures the patient is comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for several weeks after the procedure. This allows time for initial recovery, adjustment to breathing through a stoma, and monitoring for any potential complications. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for laryngectomy typically involves a thorough evaluation by a multidisciplinary team, including a head and neck surgeon, oncologist, speech therapist, and other specialists. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. Smoking should be avoided to enhance healing and reduce the risk of complications. Pre-operative tests, such as blood work, imaging studies, and possibly a biopsy, are often required to plan the surgery.Procedure Duration
The laryngectomy procedure typically takes about 5 to 12 hours, depending on the complexity of the case and whether additional procedures, such as neck dissection or reconstruction, are performed. During the surgery, the entire larynx is removed, and a stoma (a permanent opening in the neck) is created to allow the patient to breathe. If necessary, a portion of the pharynx may also be removed, and a feeding tube may be placed temporarily to assist with nutrition during the initial recovery phase.Recovery Time
Recovery from laryngectomy is a long and gradual process, with initial healing taking several weeks. Patients will need to adapt to breathing through a stoma and may require speech therapy to learn alternative methods of communication, such as esophageal speech, a voice prosthesis, or an electrolarynx. Pain management, wound care, and nutritional support are critical during the initial recovery phase. Patients may experience challenges with swallowing, mucus management, and changes in taste and smell. Full recovery, including adaptation to lifestyle changes, can take several months, and ongoing follow-up care is essential to monitor for recurrence of cancer or other complications.Estimated Cost
The cost of laryngectomy can vary widely depending on the surgeon's expertise, the complexity of the procedure, geographic location, and whether the surgery is part of a broader cancer treatment plan that includes radiation therapy or chemotherapy. The cost also includes post-operative care, rehabilitation, and potentially the need for specialized equipment, such as a voice prosthesis. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for laryngectomy involves managing the stoma, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the stoma, including cleaning and managing mucus. Speech therapy and rehabilitation are essential components of post-operative care, as patients will need to learn new ways to communicate and adapt to life without a larynx. Nutritional support, including guidance on diet and potentially the use of a feeding tube, may be necessary during the initial recovery phase. Follow-up appointments are crucial to monitor healing, assess the effectiveness of cancer treatment, and address any complications. In the case of any severe pain, fever, significant bleeding, or breathing difficulties, patients should seek immediate medical attention.
Salivary Gland Surgery
- Purpose: Removes or treats salivary glands to address infections, stones, or tumors.
- Procedure: Surgical techniques vary depending on the condition and gland involved.
-
Note: The information provided here applies to routine Salivary Gland Surgery procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the type and location of the gland involved, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the surgery, and the need for additional interventions (e.g., removal of tumors or stones) can also influence the surgery and recovery process.
Inpatient/Outpatient
Salivary Gland Surgery can be performed as either an inpatient or outpatient procedure, depending on the complexity of the surgery and the patient’s overall health. Minor procedures, such as the removal of small stones or cysts, are often done on an outpatient basis. More extensive surgeries, such as the removal of a major salivary gland (e.g., parotidectomy), may require an overnight stay for closer monitoring.Hospital Stay Duration
For minor salivary gland surgeries, patients generally do not require an overnight hospital stay and can return home the same day. For more complex procedures, such as the removal of a parotid gland or submandibular gland, a hospital stay of 1 to 2 days may be necessary to monitor for complications such as bleeding, infection, or facial nerve injury.Type of Anesthesia
Salivary Gland Surgery is usually performed under general anesthesia, meaning the patient will be fully unconscious during the procedure. In some cases, local anesthesia with sedation may be used, particularly for less invasive procedures. The choice of anesthesia depends on the patient’s preference, the extent of the surgery, and the surgeon’s recommendation.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as swelling, infection, or bleeding. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for Salivary Gland Surgery typically involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery. Smoking should be avoided to enhance healing and reduce the risk of complications. Pre-operative imaging studies, such as an ultrasound, MRI, or CT scan, may be required to assess the size and location of the gland or any associated tumors or stones.Procedure Duration
The duration of Salivary Gland Surgery varies depending on the complexity of the procedure and the gland involved. Minor procedures, such as the removal of stones or small cysts, may take 30 minutes to 1 hour. More extensive surgeries, such as a parotidectomy (removal of the parotid gland) or submandibular gland excision, may take 2 to 4 hours or longer. During the surgery, the surgeon carefully removes the affected gland or tumor, taking care to preserve surrounding structures, such as the facial nerve, which is particularly important in parotid gland surgery.Recovery Time
Recovery from Salivary Gland Surgery can take several weeks. Most patients experience swelling, bruising, and mild pain in the area where the surgery was performed. Pain management is crucial, and patients are usually prescribed pain relievers to help manage discomfort. Patients are typically advised to avoid strenuous activities, heavy lifting, and any activities that could strain the surgical area for at least 2 weeks. A soft or liquid diet may be recommended initially, especially if the surgery involved the submandibular gland or if there is difficulty swallowing. Full recovery, including the resolution of swelling and return to normal activities, can take several weeks to a few months, depending on the extent of the surgery.Estimated Cost
The cost of Salivary Gland Surgery can vary widely depending on the surgeon's expertise, the complexity of the procedure, geographic location, and whether the surgery is part of a broader treatment plan for conditions such as tumors or chronic infections. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for Salivary Gland Surgery involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the surgical site, including keeping the area clean and dry. Patients may be advised to use ice packs to reduce swelling and to avoid applying pressure to the area. Follow-up appointments are essential to monitor healing, remove any sutures, and assess the overall success of the surgery. In the case of any severe pain, fever, significant swelling, or facial weakness, patients should seek immediate medical attention.
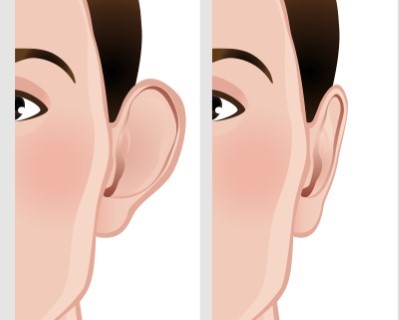
Otoplasty
- Purpose: Reshapes the ears to improve appearance or correct deformities.
- Procedure: Surgical techniques are used to modify the ear cartilage.
-
Note: The information provided here applies to routine Otoplasty procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the extent of ear reshaping needed, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Otoplasty is typically performed as an outpatient procedure, meaning most patients can return home the same day after a short observation period.Hospital Stay Duration
Patients undergoing otoplasty generally do not require an overnight hospital stay unless there are complications or specific medical concerns. The surgery usually takes about 1 to 2 hours.Type of Anesthesia
Otoplasty can be performed under local anesthesia with sedation for adults, or general anesthesia for children, to ensure comfort during the procedure.Travel After Procedure
Patients are generally able to travel shortly after the procedure, but it is advisable to rest for the remainder of the day and avoid strenuous activities. Long-distance travel should be avoided for at least 1 week.Pre-procedure Preparation
Preparation for otoplasty involves following specific guidelines provided by the healthcare provider, such as avoiding certain medications and fasting before the surgery, if general anesthesia is used.Procedure Duration
The otoplasty procedure typically takes about 1 to 2 hours. During the surgery, the surgeon reshapes the cartilage of the ears to create a more natural and aesthetically pleasing appearance. The ears are then secured in their new position with sutures.Recovery Time
Recovery from otoplasty usually takes 1 to 2 weeks. Patients may experience some swelling, bruising, and discomfort during the initial recovery period. A headband is often worn to protect the ears and maintain their new shape during healing. Most patients can return to normal activities, including work or school, within a week, but should avoid strenuous activities and contact sports for several weeks.Estimated Cost
The cost of otoplasty can vary depending on the surgeon's expertise, the complexity of the procedure, and geographic location. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for otoplasty involves managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions, which may include wearing a headband, avoiding pressure on the ears, and attending follow-up appointments to monitor healing and remove sutures.
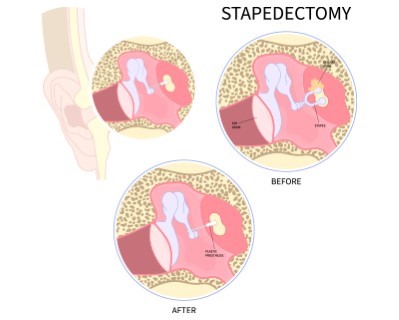
Stapedectomy
- Purpose: Treats hearing loss caused by otosclerosis by replacing the stapes bone in the middle ear.
- Procedure: The stapes bone is removed and replaced with a prosthesis.
-
Note: The information provided here applies to routine Stapedectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the extent of hearing loss, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Stapedectomy is typically performed as an outpatient procedure, meaning most patients can return home the same day after a short observation period.Hospital Stay Duration
Patients undergoing stapedectomy generally do not require an overnight hospital stay unless complications arise. The surgery typically takes about 1 to 2 hours.Type of Anesthesia
Stapedectomy is usually performed under local anesthesia with sedation, allowing the patient to remain relaxed and comfortable while still conscious. In some cases, general anesthesia may be used.Travel After Procedure
Patients are generally able to travel shortly after the procedure, though it is advisable to rest for the remainder of the day and avoid strenuous activities. Long-distance travel, particularly by air, should be avoided for at least 1 to 2 weeks to prevent pressure changes that could affect healing.Pre-procedure Preparation
Preparation for stapedectomy involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid certain medications, such as blood thinners, and to fast for a few hours before the procedure if general anesthesia is used.Procedure Duration
The stapedectomy procedure typically takes about 1 to 2 hours. During the surgery, the surgeon removes part or all of the stapes bone in the middle ear and replaces it with a prosthesis. This helps to improve hearing by allowing sound waves to be transmitted more effectively to the inner ear.Recovery Time
Recovery from stapedectomy usually takes several weeks. Patients may experience dizziness, mild pain, and a feeling of fullness in the ear during the initial recovery period. It is important to avoid activities that could strain the ear, such as heavy lifting, bending over, or flying, for several weeks. Most patients can return to light activities within a few days but should follow their surgeon’s specific guidelines for a safe recovery. Full hearing improvement may take several weeks to a few months as the ear heals.Estimated Cost
The cost of stapedectomy can vary depending on the surgeon's expertise, the complexity of the procedure, and geographic location. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for stapedectomy involves managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions, which may include avoiding getting water in the ear, avoiding loud noises, and attending follow-up appointments to monitor healing and assess hearing improvement. In the case of any severe dizziness, pain, or changes in hearing, patients should seek immediate medical attention.
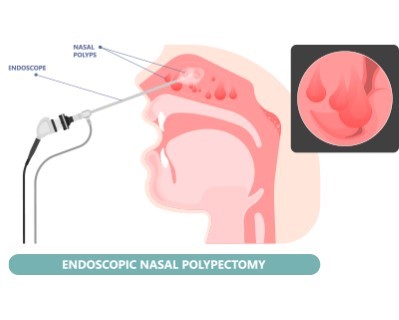
Nasal Polypectomy
- Purpose: Removes nasal polyps to improve breathing and reduce sinus infections.
- Procedure: Nasal polyps are surgically removed using endoscopic techniques.
-
Note: The information provided here applies to routine Nasal Polypectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the size and number of polyps, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Nasal Polypectomy is typically performed as an outpatient procedure, meaning most patients can return home the same day after a short observation period.Hospital Stay Duration
Patients undergoing nasal polypectomy generally do not require an overnight hospital stay unless there are complications or additional procedures involved. The surgery usually takes about 30 minutes to 1 hour, depending on the extent of the polyp removal.Type of Anesthesia
Nasal polypectomy is usually performed under local anesthesia with sedation, allowing the patient to remain relaxed and comfortable during the procedure. In some cases, general anesthesia may be used, particularly if the surgery is more extensive or if the patient prefers to be fully unconscious.Travel After Procedure
Patients are generally able to travel shortly after the procedure, though it is advisable to rest for the remainder of the day and avoid strenuous activities. Long-distance travel should be avoided for at least a few days to allow for initial recovery and to monitor for any potential complications, such as bleeding or infection.Pre-procedure Preparation
Preparation for nasal polypectomy involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid certain medications, such as blood thinners, and to fast for a few hours before the procedure if general anesthesia is used. It is also important to inform the surgical team of any allergies or previous reactions to anesthesia.Procedure Duration
The nasal polypectomy procedure typically takes about 30 minutes to 1 hour. During the surgery, the surgeon uses specialized instruments to remove the nasal polyps from the nasal passages and sinuses. In some cases, endoscopic techniques are used, which involve a thin, flexible tube with a camera to guide the removal process. The goal of the procedure is to clear the nasal passages and improve breathing, as well as to reduce symptoms such as nasal congestion, sinus pressure, and loss of smell.Recovery Time
Recovery from nasal polypectomy usually takes 1 to 2 weeks. Most patients experience mild pain, nasal congestion, and some blood-tinged discharge during the initial recovery period. Patients are typically advised to avoid strenuous activities, heavy lifting, and bending over for at least 1 week to minimize the risk of bleeding. It is also important to avoid blowing the nose forcefully during the early recovery period. Full recovery, including the resolution of nasal congestion and improvement in breathing, may take a few weeks. Follow-up appointments are necessary to monitor healing and to assess the success of the polyp removal.Estimated Cost
The cost of nasal polypectomy can vary depending on the surgeon's expertise, the complexity of the procedure, and geographic location. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for nasal polypectomy involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the nose after surgery, including using saline nasal sprays to keep the nasal passages moist and avoiding irritants such as smoke and strong odors. Follow-up appointments are essential to monitor healing, remove any packing or splints if placed, and assess the overall success of the surgery. In the case of any severe pain, fever, significant bleeding, or difficulty breathing, patients should seek immediate medical attention.
