Gastroenterology Treatments

Endoscopy
- Purpose: Examines the upper digestive system for diagnosis and treatment.
- Procedure: An endoscope, a flexible tube with a camera, is inserted through the mouth to examine the esophagus, stomach, and duodenum.
-
Note: The information provided here applies to elective endoscopy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of gastrointestinal conditions, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the type of endoscopy (upper, lower, or specialized), and the need for additional interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
Endoscopy is typically performed as an outpatient procedure. It is minimally invasive and allows most patients to return home the same day. The procedure is usually conducted in a hospital or specialized clinic, and patients are monitored for a short time afterward to ensure they recover safely from sedation.Hospital Stay Duration
Patients undergoing endoscopy generally do not require an overnight hospital stay. The procedure typically takes between 15 minutes to 1 hour, depending on the type of endoscopy being performed (e.g., upper endoscopy, colonoscopy). After the procedure, patients are monitored for a brief period to ensure they recover from sedation or anesthesia without complications, and they are usually discharged the same day.Type of Anesthesia
Endoscopy is usually performed under conscious sedation, which helps relax the patient and minimize discomfort while allowing them to remain partially awake. In some cases, particularly for longer or more complex procedures, general anesthesia may be used. Local anesthesia may also be applied to the throat if an upper endoscopy is performed.Travel After Procedure
Patients are generally advised to avoid driving and long-distance travel for the remainder of the day after the procedure, especially if sedation was used. Most patients can resume normal activities the following day, but they should follow specific recommendations from their healthcare provider regarding activity levels and travel.Pre-procedure Preparation
Preparation for endoscopy varies depending on the type of procedure. For upper endoscopy, patients are usually instructed to fast for several hours before the procedure. For colonoscopy, patients typically undergo a bowel prep the day before the procedure, which involves taking a laxative solution to clear the intestines. The healthcare provider will provide detailed instructions tailored to the specific type of endoscopy.Procedure Duration
The duration of an endoscopy procedure typically ranges from 15 minutes to 1 hour, depending on the complexity and purpose of the procedure. For example, a diagnostic upper endoscopy may take only 15-30 minutes, while a colonoscopy may take up to an hour, especially if polyps are removed or biopsies are taken.Recovery Time
Recovery from endoscopy is generally quick, with most patients able to resume light activities within a few hours after the procedure. If sedation was used, patients should rest for the remainder of the day and avoid making important decisions or operating heavy machinery. Full recovery and a return to normal activities usually occur within a day.Estimated Cost
The cost of an endoscopy can vary depending on the clinic, geographic location, and the type of endoscopy performed. Costs may also vary if additional procedures, such as biopsies or polyp removal, are performed during the endoscopy. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for endoscopy involves monitoring for any signs of complications, such as bleeding, persistent pain, or difficulty swallowing (in the case of upper endoscopy). Patients should follow any dietary recommendations provided by their healthcare provider, which may include starting with a light meal after the procedure. Follow-up appointments may be necessary to discuss biopsy results or to plan further treatment if any abnormalities were detected.

Colonoscopy
Purpose: Screens for colon cancer and diagnoses various gastrointestinal issues.Procedure: A long, flexible tube with a camera (colonoscope) is inserted through the rectum to examine the colon.
Note: The information provided here applies to elective colonoscopy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of gastrointestinal conditions, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the examination, and the need for additional interventions, such as polyp removal, can also influence the procedure and recovery process.
Inpatient/Outpatient
Colonoscopy is typically performed as an outpatient procedure. It is minimally invasive, and most patients can return home the same day. The procedure is usually conducted in a hospital or specialized clinic, and patients are monitored for a short period afterward to ensure they recover safely from sedation.
Hospital Stay Duration
Patients undergoing colonoscopy generally do not require an overnight hospital stay. The procedure itself usually takes about 30 minutes to 1 hour, depending on the findings and whether any polyps are removed or biopsies are taken. After the procedure, patients are monitored until the effects of sedation wear off, and they are usually discharged within a few hours.
Type of Anesthesia
Colonoscopy is usually performed under conscious sedation, which helps relax the patient and minimize discomfort while allowing them to remain partially awake. In some cases, deeper sedation or general anesthesia may be used, depending on the patient's preference or medical condition.
Travel After Procedure
Patients are generally advised to avoid driving and long-distance travel for the remainder of the day after the procedure, especially if sedation was used. It is recommended that patients have someone accompany them to drive them home. Most patients can resume normal activities the following day, but they should follow specific recommendations from their healthcare provider regarding activity levels and travel.
Pre-procedure Preparation
Preparation for colonoscopy involves a bowel prep to clear the intestines, which is essential for obtaining clear views during the procedure. This typically includes following a clear liquid diet the day before the procedure and taking a prescribed laxative solution to clean out the colon. Detailed instructions will be provided by the healthcare provider, and it is important for patients to follow them carefully to ensure the success of the procedure.
Procedure Duration
The colonoscopy procedure typically takes about 30 minutes to 1 hour. The duration may be longer if polyps are removed, or biopsies are taken during the examination. The colonoscope is inserted into the rectum and guided through the colon to examine the lining for any abnormalities.
Recovery Time
Recovery from colonoscopy is generally quick, with most patients able to resume light activities within a few hours after the procedure. If sedation was used, patients should rest for the remainder of the day and avoid making important decisions or operating heavy machinery. Full recovery and a return to normal activities usually occur the following day.
Estimated Cost
The cost of colonoscopy can vary depending on the clinic, geographic location, and whether any additional procedures, such as polyp removal or biopsy, are performed during the examination. For accurate cost information, patients should contact their healthcare provider or treatment center directly.
Post-procedure Care
Post-procedure care for colonoscopy includes monitoring for any signs of complications, such as persistent abdominal pain, bleeding, or fever. Patients may experience some bloating or discomfort due to air introduced into the colon during the procedure, but this usually resolves quickly. If polyps were removed or biopsies taken, patients will be given specific instructions on when to resume regular activities and diet. Follow-up appointments may be necessary to discuss the results of the colonoscopy and any further treatment if abnormalities were found.
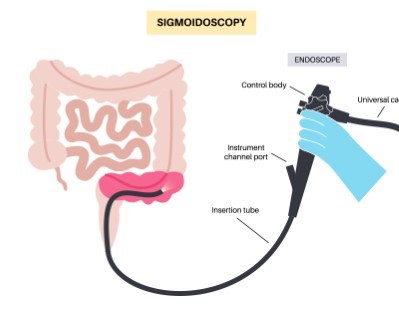
Sigmoidoscopy
- Purpose: Examines the lower part of the colon and rectum for diagnosis and screening.
- Procedure: A flexible sigmoidoscope is inserted through the rectum to visualize the lower colon.
-
Note: The information provided here applies to elective sigmoidoscopy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of gastrointestinal conditions, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the examination, and the need for additional interventions, such as biopsy or polyp removal, can also influence the procedure and recovery process.
Inpatient/Outpatient
Sigmoidoscopy is typically performed as an outpatient procedure. It is a minimally invasive procedure that allows most patients to return home the same day. The procedure is usually conducted in a hospital or specialized clinic, and patients are monitored briefly afterward to ensure they recover safely.Hospital Stay Duration
Patients undergoing sigmoidoscopy generally do not require an overnight hospital stay. The procedure itself usually takes about 10 to 20 minutes, depending on whether any biopsies or polyp removals are performed. After the procedure, patients are monitored for a short period to ensure they are stable and can usually be discharged within an hour.Type of Anesthesia
Sigmoidoscopy is often performed without the need for sedation or general anesthesia, as it is less invasive than a full colonoscopy and examines only the lower part of the colon. However, patients may be given a mild sedative or pain reliever to help minimize discomfort during the procedure.Travel After Procedure
Patients are usually able to travel shortly after the procedure, as sedation is often not required. However, if a sedative was used, patients should avoid driving and arrange for someone to take them home. Most patients can resume normal activities the same day, but they should follow specific recommendations from their healthcare provider regarding travel and activity levels.Pre-procedure Preparation
Preparation for sigmoidoscopy is generally less intensive than for a full colonoscopy. Patients may be advised to follow a clear liquid diet for a short period before the procedure and may be given an enema or laxative to clear the lower colon. The healthcare provider will provide specific instructions tailored to the patient’s needs.Procedure Duration
The sigmoidoscopy procedure typically takes about 10 to 20 minutes. The procedure involves inserting a sigmoidoscope through the rectum to examine the lower part of the colon (sigmoid colon) for abnormalities. If necessary, biopsies can be taken, and small polyps can be removed during the procedure.Recovery Time
Recovery from sigmoidoscopy is generally quick, with most patients able to return to their normal activities immediately after the procedure. If a sedative was used, patients should rest for the remainder of the day and avoid operating heavy machinery. Some patients may experience mild cramping or bloating, but this typically resolves quickly.Estimated Cost
The cost of sigmoidoscopy can vary depending on the clinic, geographic location, and whether any additional procedures, such as biopsy or polyp removal, are performed during the examination. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for sigmoidoscopy includes monitoring for any signs of complications, such as persistent abdominal pain, bleeding, or fever. Patients may experience some mild discomfort or bloating due to the air introduced into the colon during the procedure, but this usually resolves quickly. If biopsies were taken or polyps removed, patients will receive specific instructions on when to resume regular activities and diet. Follow-up appointments may be necessary to discuss the results of the sigmoidoscopy and any further treatment if abnormalities were found.

Capsule Endoscopy
- Purpose: Visualizes the small intestine to diagnose conditions like Crohn's disease, tumors, and bleeding.
- Procedure: The patient swallows a small capsule with a camera that takes pictures of the digestive tract.
-
Note: The information provided here applies to elective Capsule Endoscopy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of gastrointestinal conditions, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the examination, and the need for additional interventions or follow-up procedures can also influence the procedure and recovery process.
Inpatient/Outpatient
Capsule Endoscopy is typically performed as an outpatient procedure. It is a non-invasive diagnostic test that allows patients to complete the examination while going about their daily activities. The procedure is conducted in a hospital or specialized clinic, where patients are provided with the capsule and instructions for the procedure.Hospital Stay Duration
Patients undergoing Capsule Endoscopy generally do not require a hospital stay. The procedure involves swallowing a small, pill-sized camera that takes images of the digestive tract as it moves through the intestines. The entire process typically takes about 8 hours, during which patients can usually leave the medical facility and continue with most of their normal activities. After the procedure, patients return to the clinic to return the recording device and review the results.Type of Anesthesia
No anesthesia is required for Capsule Endoscopy. The patient simply swallows the capsule with water, and it naturally travels through the gastrointestinal tract, capturing images along the way.Travel After Procedure
Patients are free to travel and engage in light activities during the Capsule Endoscopy procedure, as it does not require sedation or anesthesia. However, patients should avoid strenuous activities, including heavy exercise, during the 8-hour recording period. They should follow specific instructions from their healthcare provider regarding any travel or activity restrictions.Pre-procedure Preparation
Preparation for Capsule Endoscopy typically involves fasting for at least 12 hours before swallowing the capsule to ensure clear images of the digestive tract. In some cases, patients may be asked to take a laxative the day before the procedure to further clear the intestines. The healthcare provider will provide specific pre-procedure instructions tailored to the patient’s needs.Procedure Duration
The Capsule Endoscopy procedure itself takes about 8 hours, during which the capsule travels through the digestive tract, capturing images. The capsule is then naturally passed in the stool, usually within 24 to 48 hours. The actual recording period for the procedure is limited to the 8-hour period after swallowing the capsule.Recovery Time
There is no recovery time needed after swallowing the capsule, and patients can usually resume normal activities immediately after the procedure is completed. Patients should ensure that the recording device remains attached during the procedure and avoid activities that could disrupt the recording.Estimated Cost
The cost of Capsule Endoscopy can vary depending on the clinic, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
After the Capsule Endoscopy, patients are typically instructed to return the recording device to their healthcare provider for analysis. There is usually no special care required after the procedure, as the capsule is naturally expelled from the body. Patients should contact their healthcare provider if they experience any unusual symptoms, such as abdominal pain or if the capsule is not passed within a few days. Follow-up appointments may be necessary to discuss the results of the endoscopy and any further treatment if abnormalities were detected.
_20240719140502236870__0.webp)
ERCP (Endoscopic Retrograde Cholangiopancreatography)
- Purpose: Diagnoses and treats conditions of the bile ducts, pancreas, and gallbladder.
- Procedure: Combines endoscopy and X-ray to examine and treat bile and pancreatic ducts.
-
Note: The information provided here applies to elective Endoscopic Retrograde Cholangiopancreatography (ERCP) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of gastrointestinal or biliary conditions, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the examination, and the need for additional interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
ERCP is typically performed as an inpatient or outpatient procedure, depending on the complexity and the patient's condition. If the procedure is straightforward and the patient is stable, they may be discharged on the same day. However, if the patient has underlying conditions or if therapeutic interventions (such as stone removal or stent placement) are performed, an overnight stay may be required for monitoring.Hospital Stay Duration
Patients undergoing ERCP may need to stay in the hospital for a few hours to a day, depending on the nature of the procedure and the patient's recovery. If the ERCP is performed for diagnostic purposes only, the stay is usually short. However, if therapeutic procedures are involved, such as removing bile duct stones or placing a stent, the hospital stay may be extended to ensure proper recovery and monitor for complications like pancreatitis or infection.Type of Anesthesia
ERCP is typically performed under conscious sedation or general anesthesia, depending on the complexity of the procedure and the patient’s overall health. Conscious sedation helps the patient remain relaxed and comfortable, while general anesthesia may be used for more complex cases or when a longer procedure is anticipated.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 24 to 48 hours after ERCP, especially if sedation or general anesthesia was used. This allows time for recovery and monitoring for any immediate complications. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels after the procedure.Pre-procedure Preparation
Preparation for ERCP typically involves fasting for at least 6 to 8 hours before the procedure to ensure the stomach is empty, reducing the risk of aspiration. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during the procedure. The healthcare provider will provide specific instructions tailored to the patient’s needs.Procedure Duration
The ERCP procedure usually takes about 30 minutes to 1 hour, depending on the complexity of the examination and whether any therapeutic interventions are performed. The procedure involves inserting an endoscope through the mouth, down the esophagus, and into the stomach and small intestine to access the bile ducts and pancreatic ducts.Recovery Time
Recovery from ERCP varies depending on the patient’s condition and the complexity of the procedure. Most patients can resume light activities within a day, but they may need to rest and avoid strenuous activities for a few days, especially if therapeutic interventions were performed. If general anesthesia was used, patients should rest for the remainder of the day and avoid making important decisions or operating heavy machinery.Estimated Cost
The cost of ERCP can vary depending on the hospital, geographic location, and whether any additional procedures, such as stent placement or stone removal, are performed. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for ERCP involves monitoring for any signs of complications, such as abdominal pain, fever, or jaundice, which could indicate pancreatitis or infection. Patients may experience mild throat discomfort due to the endoscope, but this typically resolves quickly. If stents were placed or stones removed, patients may need follow-up appointments to monitor their condition and assess the success of the procedure. Dietary restrictions and medication adjustments may also be necessary depending on the findings and interventions during the ERCP.
_20240719140514168799__0.webp)
Endoscopic Ultrasound (EUS)
- Purpose: Examines the digestive tract and surrounding tissues and organs.
- Procedure: Combines endoscopy and ultrasound to obtain images of the digestive tract and nearby structures.
-
Note: The information provided here applies to elective Endoscopic Ultrasound (EUS) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of gastrointestinal or pancreatic conditions, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the examination, and the need for additional interventions, such as biopsy or drainage, can also influence the procedure and recovery process.
Inpatient/Outpatient
Endoscopic Ultrasound (EUS) is typically performed as an outpatient procedure. This minimally invasive procedure allows most patients to return home the same day. It is often conducted in a hospital or specialized clinic, and patients are monitored briefly afterward to ensure they recover safely from sedation.Hospital Stay Duration
Patients undergoing EUS generally do not require an overnight hospital stay. The procedure itself usually takes about 30 to 90 minutes, depending on whether additional interventions, such as a fine-needle aspiration (FNA) biopsy, are performed. After the procedure, patients are monitored for a short period to ensure they are stable and can usually be discharged within a few hours.Type of Anesthesia
EUS is typically performed under conscious sedation, which helps the patient relax and minimizes discomfort while allowing them to remain partially awake. In some cases, deeper sedation or general anesthesia may be used, especially if complex interventions are anticipated or if the patient has specific health considerations.Travel After Procedure
Patients are generally advised to avoid driving and long-distance travel for the remainder of the day after the procedure, especially if sedation was used. It is recommended that patients have someone accompany them to drive them home. Most patients can resume normal activities the following day, but they should follow specific recommendations from their healthcare provider regarding travel and activity levels.Pre-procedure Preparation
Preparation for EUS typically involves fasting for at least 6 to 8 hours before the procedure to ensure the stomach is empty, reducing the risk of aspiration. Patients may also need to adjust or stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding if a biopsy is planned. The healthcare provider will provide specific pre-procedure instructions tailored to the patient’s needs.Procedure Duration
The EUS procedure typically takes about 30 to 90 minutes, depending on the complexity of the examination and whether any additional procedures, such as biopsy or drainage, are performed. The endoscope, which has an ultrasound device at its tip, is inserted through the mouth (or rectum, depending on the area being examined) to obtain detailed images of the digestive tract and surrounding organs.Recovery Time
Recovery from EUS is generally quick, with most patients able to resume light activities within a day. If sedation was used, patients should rest for the remainder of the day and avoid operating heavy machinery or making important decisions. Full recovery, including the resolution of any mild throat discomfort or bloating, usually occurs within a day or two.Estimated Cost
The cost of EUS can vary depending on the hospital, geographic location, and whether any additional procedures, such as biopsy or stent placement, are performed during the examination. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for EUS involves monitoring for any signs of complications, such as persistent abdominal pain, bleeding, or fever, which could indicate a rare complication like infection or perforation. Patients may experience mild throat discomfort due to the endoscope, but this typically resolves quickly. If a biopsy was performed, patients may receive additional instructions regarding activity levels and dietary restrictions. Follow-up appointments may be necessary to discuss the results of the EUS and any further treatment if abnormalities were detected.
Liver Biopsy
- Purpose: Diagnoses liver diseases by examining liver tissue samples.
- Procedure: A needle is inserted through the skin to remove a small piece of liver tissue for analysis.
-
Note: The information provided here applies to elective liver biopsy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of liver disease, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the type of biopsy (percutaneous, transjugular, or laparoscopic), and the need for additional interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
Liver biopsy is typically performed as an outpatient procedure. Depending on the type of biopsy and the patient's overall condition, most patients can return home the same day after a few hours of observation. However, in some cases, particularly if there are concerns about bleeding or if the patient has other underlying conditions, a short hospital stay might be required for closer monitoring.Hospital Stay Duration
Patients undergoing liver biopsy generally do not require an overnight hospital stay, but they are monitored for a few hours after the procedure to ensure there are no immediate complications, such as bleeding or severe pain. The actual procedure takes about 15 to 30 minutes, but the total time spent at the facility may be several hours to allow for preparation, the procedure itself, and recovery.Type of Anesthesia
Liver biopsy is typically performed under local anesthesia, which numbs the area where the biopsy needle will be inserted. In some cases, conscious sedation may be used to help the patient relax. If a transjugular or laparoscopic approach is used, general anesthesia may be required, especially if the procedure is performed in conjunction with other interventions.Travel After Procedure
Patients are generally advised to avoid driving and long-distance travel for at least 24 hours after the procedure, especially if sedation or anesthesia was used. Most patients can resume normal activities the next day, but they should follow specific recommendations from their healthcare provider regarding travel and physical activity.Pre-procedure Preparation
Preparation for a liver biopsy typically involves fasting for 6 to 8 hours before the procedure. Patients may need to stop taking certain medications, particularly blood thinners, a few days before the biopsy to reduce the risk of bleeding. A blood test may be performed before the procedure to check the patient's clotting status. The healthcare provider will provide detailed pre-procedure instructions tailored to the patient’s needs.Procedure Duration
The liver biopsy procedure typically takes about 15 to 30 minutes. The most common approach is percutaneous, where a needle is inserted through the skin into the liver to obtain a tissue sample. Transjugular and laparoscopic biopsies are less common and may take longer, depending on the complexity of the procedure.Recovery Time
Recovery from a liver biopsy is generally quick, with most patients able to return to light activities within 24 hours. However, patients are usually advised to avoid strenuous activities, heavy lifting, and alcohol consumption for several days to minimize the risk of bleeding or other complications. Patients should rest for the remainder of the day after the procedure.Estimated Cost
The cost of a liver biopsy can vary depending on the hospital, geographic location, and the type of biopsy performed. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for liver biopsy involves monitoring for signs of complications, such as severe pain, bleeding, or signs of infection at the biopsy site. Patients should follow their healthcare provider’s instructions on how to care for the biopsy site and any activity restrictions. Follow-up appointments may be necessary to review the biopsy results and discuss any further treatment if liver disease or other abnormalities were detected.
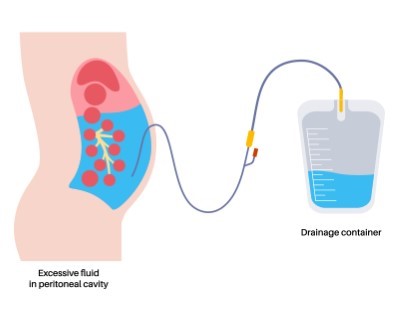
Paracentesis
- Purpose: Removes excess fluid from the abdominal cavity to diagnose or relieve symptoms.
- Procedure: A needle is inserted into the abdomen to drain the fluid.
-
Note: The information provided here applies to elective paracentesis procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the underlying cause of ascites (abdominal fluid accumulation), patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the volume of fluid to be drained, and the need for additional interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
Paracentesis is typically performed as an outpatient procedure. It is a minimally invasive procedure that allows most patients to return home the same day. In some cases, particularly if a large volume of fluid is removed or if the patient has underlying health concerns, a short observation period or hospital stay might be necessary.Hospital Stay Duration
Patients undergoing paracentesis generally do not require an overnight hospital stay. The procedure itself usually takes about 20 to 45 minutes, depending on the amount of fluid being removed. After the procedure, patients are monitored for a short period to ensure they are stable and can usually be discharged within a few hours.Type of Anesthesia
Paracentesis is typically performed under local anesthesia, which numbs the area where the needle or catheter is inserted. This ensures that the patient is comfortable during the procedure. Sedation is not usually required, but in some cases, mild sedation may be offered if the patient is particularly anxious.Travel After Procedure
Patients are generally able to travel shortly after the procedure, although it is advised to avoid strenuous activities or heavy lifting for the remainder of the day. Light activities can usually be resumed the following day. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels.Pre-procedure Preparation
Preparation for paracentesis is generally straightforward. Patients may be advised to avoid eating or drinking for a few hours before the procedure, particularly if there is a risk of sedation being used. In some cases, a blood test may be performed beforehand to check clotting ability. The healthcare provider will provide specific instructions tailored to the patient’s needs.Procedure Duration
The paracentesis procedure typically takes about 20 to 45 minutes. During the procedure, a needle or catheter is inserted through the abdominal wall into the peritoneal cavity to drain the accumulated fluid. The amount of fluid removed can vary, and in cases where large volumes are drained, the procedure may take longer.Recovery Time
Recovery from paracentesis is generally quick, with most patients able to resume normal activities within a day. Patients are usually advised to rest for the remainder of the day after the procedure and avoid any strenuous activities. If a large volume of fluid was removed, patients may feel fatigued and should ensure adequate hydration and rest.Estimated Cost
The cost of paracentesis can vary depending on the clinic, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for paracentesis includes monitoring the puncture site for signs of infection, bleeding, or fluid leakage. Patients should also be aware of symptoms such as dizziness, weakness, or abdominal pain, which could indicate complications. Follow-up appointments may be necessary to monitor the underlying condition causing the fluid accumulation and to plan any further treatment. Patients will receive instructions on how to care for the puncture site and any activity restrictions needed during recovery.
_20240719140548121634__0.webp)
Percutaneous Endoscopic Gastrostomy (PEG)
- Purpose: Provides long-term feeding access for patients unable to eat orally.
- Procedure: A feeding tube is placed through the abdominal wall into the stomach using an endoscope.
-
Note: The information provided here applies to elective Percutaneous Endoscopic Gastrostomy (PEG) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the underlying medical condition necessitating the PEG, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the placement, and the need for additional interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
PEG is typically performed as an inpatient or outpatient procedure, depending on the patient’s condition and the reason for the tube placement. For patients who are stable and not critically ill, the procedure may be done on an outpatient basis, allowing them to return home the same day after a short observation period. However, if the patient has significant medical issues or if the procedure is complex, a short hospital stay may be required.Hospital Stay Duration
For patients undergoing PEG as an outpatient procedure, the hospital stay is usually limited to a few hours for observation after the procedure. If the procedure is done on an inpatient basis, the stay may last 1 to 2 days, or longer if complications arise or if the patient needs additional care for their underlying condition.Type of Anesthesia
PEG is typically performed under conscious sedation combined with local anesthesia to numb the area where the tube will be inserted. This approach helps to keep the patient comfortable and relaxed while still allowing them to follow instructions during the procedure. In some cases, general anesthesia may be used, particularly if the patient is unable to tolerate sedation or if the procedure is complex.Travel After Procedure
Patients are generally advised to avoid travel for at least 24 to 48 hours after the procedure, particularly if sedation or anesthesia was used. This allows time for initial recovery and monitoring for any early complications, such as pain, bleeding, or infection. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels after the procedure.Pre-procedure Preparation
Preparation for PEG typically involves fasting for at least 6 to 8 hours before the procedure to ensure an empty stomach, which reduces the risk of complications. Patients may also need to adjust or stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during the procedure. The healthcare provider will provide specific instructions tailored to the patient’s needs.Procedure Duration
The PEG procedure typically takes about 30 to 60 minutes. During the procedure, an endoscope is passed through the mouth and into the stomach to visualize the placement site. A small incision is made in the abdomen, and the feeding tube is placed directly into the stomach through this incision.Recovery Time
Recovery from PEG placement varies, but most patients can resume light activities within a few days. Patients should follow specific instructions on how to care for the PEG site, including how to clean and manage the tube. It is essential to monitor for any signs of infection, such as redness, swelling, or discharge around the tube site. Full recovery, including adapting to feeding through the tube, may take a few weeks, during which time patients should follow their healthcare provider’s guidance.Estimated Cost
The cost of PEG placement can vary depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for PEG involves daily cleaning and maintenance of the tube site to prevent infection. Patients and caregivers will receive detailed instructions on how to use and care for the feeding tube, including how to administer feedings and medications through the tube. Regular follow-up appointments are necessary to monitor the PEG site, assess nutritional status, and address any complications that may arise. Patients should be aware of signs of potential complications, such as pain, leakage, or blockages in the tube, and report these to their healthcare provider promptly.

Colorectal Cancer Screening
- Purpose: Detects colorectal cancer at an early, more treatable stage.
- Procedure: Various methods such as colonoscopy, sigmoidoscopy, and stool tests are used for screening.
-
Note: The information provided here applies to elective colorectal cancer screening under standard conditions. However, specifics may vary depending on individual patient factors, such as age, family history, personal medical history, or any complications that might arise during or after the screening procedure. The patient’s overall health, the type of screening test chosen, and the need for additional interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
Colorectal cancer screening is typically performed as an outpatient procedure. Most screening tests, including colonoscopy, sigmoidoscopy, and stool-based tests, do not require hospital admission and allow patients to return home the same day.Hospital Stay Duration
Patients undergoing colorectal cancer screening generally do not require an overnight hospital stay. If a colonoscopy is chosen as the screening method, the procedure typically takes about 30 minutes to 1 hour, followed by a short recovery period to allow the effects of sedation to wear off. Patients are usually discharged within a few hours after the procedure. For stool-based tests, no hospital stay is required, as these tests are often done at home.Type of Anesthesia
The type of anesthesia used depends on the screening method. Colonoscopy is usually performed under conscious sedation or, in some cases, general anesthesia, to keep the patient comfortable during the procedure. Sigmoidoscopy may be performed without sedation or with mild sedation. Stool-based tests, such as the fecal immunochemical test (FIT) or stool DNA test, do not require any anesthesia.Travel After Procedure
Patients undergoing colonoscopy are advised to avoid driving and long-distance travel for the remainder of the day after the procedure, especially if sedation was used. It is recommended that patients have someone accompany them to drive them home. Most patients can resume normal activities the following day, but they should follow specific recommendations from their healthcare provider regarding travel and activity levels. For stool-based tests, there are no travel restrictions.Pre-procedure Preparation
Preparation for colorectal cancer screening depends on the type of test. For colonoscopy, patients typically need to follow a clear liquid diet and take a bowel preparation solution to cleanse the colon the day before the procedure. Specific instructions will be provided by the healthcare provider. For sigmoidoscopy, the preparation is usually less extensive but may still involve a cleansing enema. Stool-based tests generally require no special preparation, but patients should follow any instructions provided with the test kit.Procedure Duration
The duration of the colorectal cancer screening procedure varies by test type. Colonoscopy typically takes 30 minutes to 1 hour, while sigmoidoscopy may take 10 to 20 minutes. Stool-based tests are done at home and require only a few minutes to complete the sample collection.Recovery Time
Recovery from a colonoscopy is generally quick, with most patients able to resume light activities within a day. If sedation was used, patients should rest for the remainder of the day and avoid operating heavy machinery. Sigmoidoscopy also has a quick recovery time, and most patients can resume normal activities shortly after the procedure. There is no recovery time required for stool-based tests.Estimated Cost
The cost of colorectal cancer screening can vary depending on the screening method, clinic, geographic location, and whether any additional procedures, such as polyp removal or biopsy, are performed. Colonoscopy tends to be the most expensive option, while stool-based tests are generally less costly. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for colorectal cancer screening depends on the test performed. After a colonoscopy or sigmoidoscopy, patients should monitor for any signs of complications, such as abdominal pain, bleeding, or fever. If polyps were removed or biopsies taken, patients may receive additional instructions regarding activity levels and dietary restrictions. Follow-up appointments may be necessary to discuss the results of the screening and any further treatment if abnormalities were detected. For stool-based tests, patients will be informed of the results and advised on any necessary follow-up steps if the test is positive.
Balloon Enteroscopy
- Purpose: Examines the small intestine for diagnosis and treatment of various conditions.
- Procedure: An endoscope with an inflatable balloon is used to navigate the small intestine.
-
Note: The information provided here applies to elective balloon enteroscopy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of gastrointestinal conditions, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the examination, and the need for additional interventions, such as biopsy or polyp removal, can also influence the procedure and recovery process.
Inpatient/Outpatient
Balloon enteroscopy is typically performed as an outpatient procedure. This advanced endoscopic technique allows most patients to return home the same day after a short observation period. However, in more complex cases or if therapeutic interventions are performed, an overnight hospital stay may be required for closer monitoring.Hospital Stay Duration
Patients undergoing balloon enteroscopy generally do not require an overnight hospital stay, unless complications arise or additional interventions are performed. The procedure itself usually takes about 1 to 3 hours, depending on the area of the small intestine being examined and whether any therapeutic procedures are performed. After the procedure, patients are monitored for a few hours to ensure they recover from sedation and are stable for discharge.Type of Anesthesia
Balloon enteroscopy is typically performed under conscious sedation or general anesthesia, depending on the complexity of the procedure and the patient’s overall health. Conscious sedation helps the patient remain relaxed and comfortable, while general anesthesia may be used for more extensive procedures or when deeper sedation is required.Travel After Procedure
Patients are generally advised to avoid driving and long-distance travel for at least 24 hours after the procedure, especially if sedation or anesthesia was used. It is recommended that patients have someone accompany them to drive them home. Most patients can resume normal activities the following day, but they should follow specific recommendations from their healthcare provider regarding travel and activity levels.Pre-procedure Preparation
Preparation for balloon enteroscopy typically involves fasting for at least 8 hours before the procedure to ensure the stomach and small intestine are empty, reducing the risk of complications. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding if biopsies or therapeutic interventions are planned. The healthcare provider will provide specific pre-procedure instructions tailored to the patient’s needs.Procedure Duration
The duration of the balloon enteroscopy procedure typically ranges from 1 to 3 hours, depending on the complexity of the examination and whether any therapeutic interventions, such as polyp removal or biopsy, are performed. The procedure involves inserting an endoscope equipped with one or two balloons into the digestive tract. The balloons are inflated and deflated to move the endoscope through the small intestine for detailed examination and treatment.Recovery Time
Recovery from balloon enteroscopy is generally quick, with most patients able to resume light activities within a day. If sedation or anesthesia was used, patients should rest for the remainder of the day and avoid operating heavy machinery or making important decisions. Full recovery and resolution of any mild discomfort, such as bloating or gas, typically occur within a day or two.Estimated Cost
The cost of balloon enteroscopy can vary depending on the hospital, geographic location, and whether any additional procedures, such as biopsy or therapeutic interventions, are performed. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for balloon enteroscopy involves monitoring for any signs of complications, such as persistent abdominal pain, bleeding, or fever. Patients may experience mild bloating or discomfort due to the air or gas used during the procedure, but this typically resolves quickly. If biopsies were taken or therapeutic interventions were performed, patients may receive additional instructions regarding activity levels and dietary restrictions. Follow-up appointments may be necessary to discuss the results of the procedure and any further treatment if abnormalities were detected.
_20240719140624337360__0.webp)
Hepatobiliary Scintigraphy (HIDA Scan)
- Purpose: Evaluates the function of the liver, gallbladder, and bile ducts.
- Procedure: A radioactive tracer is injected, and a special camera takes images of the liver, gallbladder, and bile ducts.
-
Note: The information provided here applies to elective Hepatobiliary Scintigraphy (HIDA Scan) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of liver or gallbladder conditions, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the scan, and the need for additional interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
Hepatobiliary Scintigraphy, commonly known as a HIDA scan, is typically performed as an outpatient procedure. This nuclear medicine imaging test allows most patients to return home the same day. The procedure is conducted in a hospital or specialized imaging center, where patients are monitored briefly afterward to ensure there are no immediate reactions to the radiotracer used.Hospital Stay Duration
Patients undergoing a HIDA scan generally do not require a hospital stay. The entire process, including preparation, the scan itself, and post-scan monitoring, usually takes about 1 to 2 hours. After the scan, patients are observed for a short period to ensure they are stable and can usually be discharged the same day.Type of Anesthesia
Anesthesia is not required for a HIDA scan. The procedure is non-invasive, involving the injection of a radioactive tracer that travels to the liver, gallbladder, and bile ducts, allowing for imaging of these structures. Patients are awake and fully alert during the procedure.Travel After Procedure
Patients are generally able to travel and resume normal activities shortly after the procedure, as there is no sedation involved. However, it is advised to follow any specific instructions from the healthcare provider, particularly regarding hydration, as it helps to flush the radioactive tracer from the body.Pre-procedure Preparation
Preparation for a HIDA scan may involve fasting for several hours before the procedure to ensure accurate results, as food can affect the functioning of the gallbladder. Patients should inform their healthcare provider about all medications they are taking, as certain drugs may need to be adjusted or paused temporarily before the scan. The healthcare provider will provide specific pre-procedure instructions tailored to the patient’s needs.Procedure Duration
The HIDA scan procedure typically takes about 1 to 2 hours. After the injection of the radiotracer, patients lie still on an imaging table while a gamma camera takes images of the tracer as it moves through the liver, gallbladder, bile ducts, and small intestine. In some cases, additional imaging may be required, extending the duration of the procedure.Recovery Time
Recovery from a HIDA scan is immediate, as the procedure is non-invasive and does not involve sedation or anesthesia. Most patients can resume normal activities and diet immediately after the procedure. It is recommended to drink plenty of fluids to help eliminate the radioactive tracer from the body.Estimated Cost
The cost of a HIDA scan can vary depending on the hospital, geographic location, and whether any additional imaging or follow-up tests are required. For accurate cost information, patients should contact their healthcare provider or imaging center directly.Post-procedure Care
Post-procedure care for a HIDA scan is minimal. Patients should monitor for any unusual symptoms, such as rash or swelling at the injection site, though these are rare. Drinking plenty of fluids after the procedure is advised to help clear the tracer from the body. Follow-up appointments may be necessary to discuss the results of the scan and any further treatment if abnormalities were detected.