General Surgery Treatments

Cholecystectomy
- Purpose: Removes the gallbladder to treat gallstones and other gallbladder diseases.
- Procedure: The gallbladder is surgically removed, typically using laparoscopic techniques.
-
Note: The information provided here applies to routine Cholecystectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of gallstones, inflammation, or other complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Cholecystectomy is typically performed as an outpatient procedure, particularly when done laparoscopically, meaning most patients can return home the same day. However, in cases of open cholecystectomy or if complications arise, an overnight hospital stay may be required for closer monitoring.Hospital Stay Duration
For laparoscopic cholecystectomy, patients usually do not require an overnight hospital stay and can be discharged within a few hours after the procedure. If an open cholecystectomy is performed, or if complications occur, a hospital stay of 2 to 3 days may be necessary.Type of Anesthesia
Cholecystectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. This ensures the patient is comfortable and allows the surgical team to perform the procedure safely.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as infection or bleeding. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for cholecystectomy involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery. Pre-operative tests, such as blood work and imaging studies (e.g., ultrasound), are often required to assess the gallbladder and plan the surgery.Procedure Duration
The cholecystectomy procedure typically takes about 1 to 2 hours. During a laparoscopic cholecystectomy, the surgeon makes several small incisions in the abdomen and uses a camera and specialized instruments to remove the gallbladder. In cases where laparoscopic surgery is not possible or safe, an open cholecystectomy may be performed, which involves a larger incision to access and remove the gallbladder.Recovery Time
Recovery from laparoscopic cholecystectomy is generally quicker, with most patients able to resume light activities within a few days and return to work within 1 to 2 weeks. For open cholecystectomy, recovery may take longer, with patients typically needing 4 to 6 weeks to fully recover. Patients are advised to avoid heavy lifting, strenuous activities, and high-fat foods during the recovery period. It is important to follow the healthcare provider’s dietary recommendations and attend follow-up appointments to monitor healing.Estimated Cost
The cost of cholecystectomy can vary depending on the surgeon's expertise, the complexity of the procedure (laparoscopic vs. open), and geographic location. Insurance coverage may also affect the out-of-pocket cost. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for cholecystectomy involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the surgical incisions, including keeping them clean and dry. Patients should also be aware of potential complications, such as infection, bleeding, or digestive issues, and seek medical attention if any concerning symptoms arise. A follow-up appointment is typically scheduled within a few weeks to assess the healing process and address any questions or concerns.

Hernia Repair
- Purpose: Repairs hernias to prevent complications and relieve symptoms.
- Procedure: The protruding tissue is pushed back into place and the weakened area is reinforced with mesh.
-
Note: The information provided here applies to routine Hernia Repair procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the size and location of the hernia, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Hernia repair is typically performed as an outpatient procedure, meaning most patients can return home the same day after a short observation period. However, in cases of complex or recurrent hernias, or if complications arise, an overnight hospital stay may be required for closer monitoring.Hospital Stay Duration
Patients undergoing hernia repair usually do not require an overnight hospital stay and can be discharged within a few hours after the procedure, once they are fully awake and stable. If an open hernia repair or a more complex procedure is performed, a hospital stay of 1 to 2 days may be necessary.Type of Anesthesia
Hernia repair can be performed under general anesthesia, local anesthesia with sedation, or spinal anesthesia, depending on the type of hernia, the complexity of the surgery, and the patient’s preference. General anesthesia is more common for laparoscopic repairs, while local or spinal anesthesia may be used for simpler, open procedures.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for any potential complications, such as infection or recurrence of the hernia. Patients should follow specific recommendations from their healthcare provider regarding travel and activity levels based on their recovery progress.Pre-procedure Preparation
Preparation for hernia repair involves following specific guidelines provided by the healthcare provider. Patients may be advised to avoid eating or drinking for several hours before the surgery, typically after midnight the night before the procedure. It is also important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery. Pre-operative tests, such as blood work and imaging studies, may be required to assess the hernia and plan the surgery.Procedure Duration
The hernia repair procedure typically takes about 30 minutes to 2 hours, depending on the complexity of the hernia and the type of repair (laparoscopic or open). During the surgery, the surgeon pushes the protruding tissue back into place and repairs the weakness in the muscle or abdominal wall, often reinforcing the area with a synthetic mesh to prevent recurrence. Laparoscopic surgery involves small incisions and the use of a camera and specialized instruments, while open surgery involves a larger incision to access and repair the hernia.Recovery Time
Recovery from hernia repair varies depending on the type of surgery performed. For laparoscopic hernia repair, most patients can resume light activities within a few days and return to work within 1 to 2 weeks. For open hernia repair, recovery may take longer, with patients typically needing 4 to 6 weeks to fully recover. Patients are advised to avoid heavy lifting, strenuous activities, and bending over during the recovery period to prevent strain on the repair site. It is important to follow the healthcare provider’s instructions on activity restrictions and attend follow-up appointments to monitor healing.Estimated Cost
The cost of hernia repair can vary depending on the surgeon's expertise, the complexity of the procedure (laparoscopic vs. open), and geographic location. Insurance coverage may also affect the out-of-pocket cost. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for hernia repair involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. It is important to follow the healthcare provider’s instructions on how to care for the surgical incisions, including keeping them clean and dry. Patients should also be aware of potential complications, such as infection, bleeding, or hernia recurrence, and seek medical attention if any concerning symptoms arise. A follow-up appointment is typically scheduled within a few weeks to assess the healing process and address any questions or concerns.
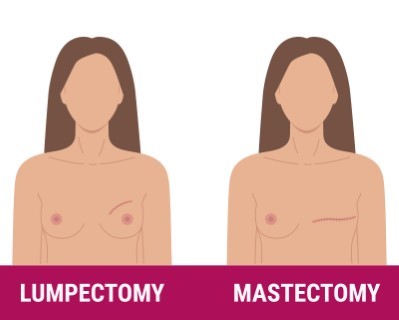
Mastectomy
- Purpose: Removes breast tissue to treat or prevent breast cancer.
- Procedure: The breast tissue is surgically removed, and reconstructive surgery may follow.
-
Note: The information provided here applies to routine Mastectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the type of breast cancer, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Mastectomy is typically performed as an inpatient procedure. Most patients require a hospital stay of 1 to 2 days for monitoring and initial recovery.Hospital Stay Duration
Patients usually stay in the hospital for 1 to 2 days after a mastectomy. If reconstruction is performed simultaneously, the stay may be longer.Type of Anesthesia
Mastectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications.Pre-procedure Preparation
Preparation for mastectomy involves following specific guidelines provided by the healthcare provider, including fasting before surgery and possibly adjusting medications. Pre-operative tests, such as blood work and imaging studies, may be required.Procedure Duration
The mastectomy procedure typically takes about 2 to 3 hours. During the surgery, the surgeon removes breast tissue, and sometimes lymph nodes, depending on the extent of the cancer. Reconstruction, if planned, can extend the surgery time.Recovery Time
Recovery from mastectomy varies, with most patients able to resume light activities within a few days and normal activities within 4 to 6 weeks. Patients should avoid strenuous activities and follow their healthcare provider’s instructions on wound care and activity restrictions.Estimated Cost
The cost of mastectomy can vary widely based on the type of mastectomy, surgeon’s expertise, geographic location, and whether reconstruction is performed. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care involves managing pain, preventing infection, and ensuring proper healing. Patients should follow their healthcare provider’s instructions on caring for surgical incisions, managing drainage tubes, and attending follow-up appointments to monitor recovery. It is also important to report any signs of complications, such as infection or lymphedema, promptly.

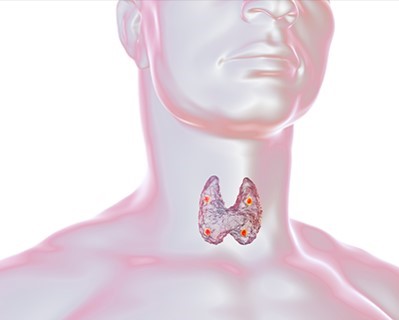
Thyroidectomy
- Purpose: Removes part or all of the thyroid gland to treat thyroid disorders.
- Procedure: The thyroid gland is surgically removed through an incision in the neck.
-
Note: The information provided here applies to routine Thyroidectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the extent of thyroid disease, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Thyroidectomy is typically performed as an inpatient procedure, although in some cases it may be done as an outpatient procedure, especially if the surgery is straightforward and there are no complications. Most patients stay in the hospital for 1 to 2 days for monitoring.Hospital Stay Duration
Patients usually stay in the hospital for 1 to 2 days after a thyroidectomy. If complications arise or if the surgery is complex, the stay may be extended.Type of Anesthesia
Thyroidectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications.Pre-procedure Preparation
Preparation for thyroidectomy involves following specific guidelines provided by the healthcare provider, including fasting before surgery and possibly adjusting medications, especially thyroid or blood-thinning medications. Pre-operative tests, such as blood work and imaging studies, are usually required.Procedure Duration
The thyroidectomy procedure typically takes about 2 to 3 hours. During the surgery, the surgeon removes part or all of the thyroid gland, depending on the condition being treated, such as thyroid cancer, nodules, or hyperthyroidism.Recovery Time
Recovery from thyroidectomy varies, with most patients able to resume light activities within a few days and normal activities within 1 to 2 weeks. Patients should avoid strenuous activities and heavy lifting during the initial recovery period. It’s important to follow the healthcare provider’s instructions on activity restrictions and wound care.Estimated Cost
The cost of thyroidectomy can vary based on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments are required. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care involves managing pain, preventing infection, and ensuring proper healing. Patients may need to take thyroid hormone replacement therapy if the entire thyroid is removed. Regular follow-up appointments are necessary to monitor hormone levels, adjust medication, and ensure proper healing. It is also important to watch for signs of complications, such as changes in voice, calcium levels, or signs of infection, and report them promptly.
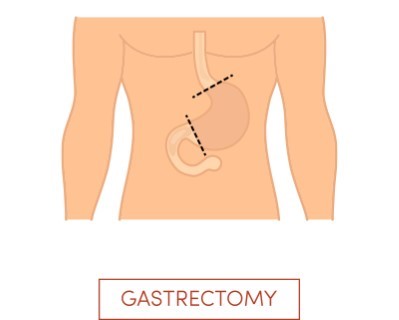
Gastrectomy
- Purpose: Removes part or all of the stomach to treat stomach cancer, ulcers, or other conditions.
- Procedure: The affected portion of the stomach is surgically removed.
-
Note: The information provided here applies to routine Gastrectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the extent of the surgery (partial or total gastrectomy), the underlying condition being treated, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Gastrectomy is typically performed as an inpatient procedure, requiring a hospital stay for monitoring and initial recovery. The length of stay depends on the extent of the surgery and the patient’s overall condition.Hospital Stay Duration
Patients undergoing gastrectomy usually stay in the hospital for 5 to 10 days, depending on the complexity of the surgery (partial or total gastrectomy) and how well the patient is recovering. Longer stays may be necessary if complications arise.Type of Anesthesia
Gastrectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications.Pre-procedure Preparation
Preparation for gastrectomy involves following specific guidelines provided by the healthcare provider, including fasting before surgery and possibly adjusting medications. Pre-operative tests, such as blood work, imaging studies, and nutritional assessments, are often required.Procedure Duration
The gastrectomy procedure typically takes about 2 to 5 hours, depending on whether a partial or total gastrectomy is being performed. During the surgery, part or all of the stomach is removed, and the digestive tract is reconnected to allow food to pass through the remaining sections.Recovery Time
Recovery from gastrectomy varies, with most patients needing several weeks to a few months to fully recover. Initial recovery in the hospital involves managing pain, gradually reintroducing liquids and foods, and monitoring for complications. Patients are typically advised to avoid strenuous activities and follow a specific dietary plan as they adjust to changes in digestion.Estimated Cost
The cost of gastrectomy can vary based on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments, such as chemotherapy, are required. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for gastrectomy involves managing pain, preventing infection, and ensuring proper healing. Patients will need to follow a specialized diet, often starting with liquids and gradually progressing to solid foods. Nutritional support, including vitamin and mineral supplementation, may be necessary, especially after a total gastrectomy. Regular follow-up appointments are essential to monitor recovery, manage any complications, and adjust dietary plans. It is important to report any signs of complications, such as difficulty eating, significant weight loss, or signs of infection, promptly.
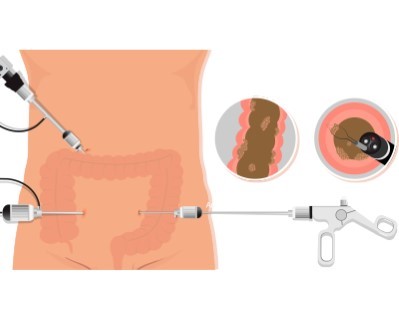
Colectomy
- Purpose: Removes part or all of the colon to treat colon cancer, Crohn's disease, or ulcerative colitis.
- Procedure: The affected portion of the colon is surgically removed.
-
Note: The information provided here applies to routine Colectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the extent of the surgery (partial or total colectomy), the underlying condition being treated, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Colectomy is typically performed as an inpatient procedure, requiring a hospital stay for monitoring and initial recovery. The length of stay depends on the extent of the surgery and the patient’s overall condition.Hospital Stay Duration
Patients undergoing colectomy usually stay in the hospital for 5 to 7 days, depending on the complexity of the surgery and how well the patient is recovering. Longer stays may be necessary if complications arise or if the patient requires more intensive post-operative care.Type of Anesthesia
Colectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications.Pre-procedure Preparation
Preparation for colectomy involves following specific guidelines provided by the healthcare provider. This may include fasting before surgery, bowel preparation to clean the intestines, and possibly adjusting medications, particularly blood thinners. Pre-operative tests, such as blood work and imaging studies, are often required.Procedure Duration
The colectomy procedure typically takes about 2 to 4 hours, depending on whether a partial or total colectomy is being performed. During the surgery, the surgeon removes the affected portion of the colon and reconnects the remaining sections. In some cases, a temporary or permanent stoma (an opening on the abdomen for waste to pass) may be created.Recovery Time
Recovery from colectomy varies, with most patients needing several weeks to a few months to fully recover. Initial recovery in the hospital involves managing pain, gradually reintroducing liquids and foods, and monitoring for complications such as infection, leakage, or bowel obstruction. Patients are typically advised to avoid strenuous activities and follow a specific dietary plan as they adjust to changes in bowel function.Estimated Cost
The cost of colectomy can vary based on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments, such as chemotherapy or radiation, are required. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for colectomy involves managing pain, preventing infection, and ensuring proper healing. Patients will need to follow a specific diet, often starting with liquids and gradually progressing to solid foods. If a stoma is created, patients will receive education on stoma care and management. Regular follow-up appointments are essential to monitor recovery, manage any complications, and adjust the treatment plan as needed. It is important to report any signs of complications, such as fever, severe pain, or changes in bowel habits, promptly.

Splenectomy
- Purpose: Removes the spleen to treat conditions such as splenic rupture, cancer, or blood disorders.
- Procedure: The spleen is surgically removed through an incision in the abdomen.
Note: The information provided here applies to routine Splenectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the underlying reason for the surgery (e.g., trauma, blood disorders, or cancer), patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Splenectomy is typically performed as an inpatient procedure, requiring a hospital stay for monitoring and initial recovery. The length of stay depends on whether the surgery is performed laparoscopically (minimally invasive) or as an open procedure, as well as the patient’s overall condition.Hospital Stay Duration
Patients undergoing laparoscopic splenectomy usually stay in the hospital for 2 to 3 days, while those who undergo an open splenectomy may require a longer stay, typically 4 to 7 days, depending on recovery progress and any complications.Type of Anesthesia
Splenectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications, such as infection or bleeding.Pre-procedure Preparation
Preparation for splenectomy involves following specific guidelines provided by the healthcare provider. Patients may be advised to fast before surgery and adjust any medications, particularly blood thinners. Pre-operative vaccinations against certain infections, such as pneumococcus, meningococcus, and Haemophilus influenzae type b (Hib), are often recommended to reduce the risk of post-splenectomy infections.Procedure Duration
The splenectomy procedure typically takes about 2 to 4 hours. During the surgery, the spleen is removed either laparoscopically, using small incisions and specialized instruments, or through an open approach with a larger incision. The choice of technique depends on the patient’s condition and the surgeon’s assessment.Recovery Time
Recovery from splenectomy varies, with most patients needing several weeks to fully recover. Patients are advised to avoid strenuous activities and heavy lifting for at least 4 to 6 weeks. Gradual return to normal activities is recommended, with close monitoring for signs of infection or other complications.Estimated Cost
The cost of splenectomy can vary depending on the surgeon's expertise, the complexity of the procedure (laparoscopic vs. open), geographic location, and whether additional treatments are required. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for splenectomy involves managing pain, preventing infection, and ensuring proper healing. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. Regular follow-up appointments are essential to monitor recovery and manage any complications. Since the spleen plays a role in immune function, patients may be more susceptible to infections and should follow their healthcare provider’s recommendations for vaccinations and preventive care. It is important to report any signs of infection, such as fever, chills, or unusual pain, promptly.

Liver Resection
- Purpose: Removes part of the liver to treat liver cancer or other liver diseases.
- Procedure: The affected portion of the liver is surgically removed.
-
Note: The information provided here applies to routine Liver Resection procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the size and location of the liver tumor, the underlying liver condition, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Liver resection is typically performed as an inpatient procedure, requiring a hospital stay for close monitoring and initial recovery. The length of the hospital stay depends on the extent of the surgery and the patient’s overall condition.Hospital Stay Duration
Patients undergoing liver resection usually stay in the hospital for 5 to 10 days, depending on the complexity of the surgery and the patient’s recovery progress. Longer stays may be necessary if complications arise.Type of Anesthesia
Liver resection is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 4 to 6 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications such as bleeding, infection, or liver dysfunction.Pre-procedure Preparation
Preparation for liver resection involves following specific guidelines provided by the healthcare provider. Patients may be advised to fast before surgery, adjust certain medications, and undergo pre-operative tests such as blood work, imaging studies, and liver function tests. A thorough evaluation by the surgical team is necessary to plan the surgery and manage any risks.Procedure Duration
The liver resection procedure typically takes about 3 to 5 hours, depending on the size and location of the portion of the liver being removed. The surgery involves removing the affected part of the liver while preserving as much healthy tissue as possible. In some cases, additional procedures, such as the removal of nearby lymph nodes, may be performed.Recovery Time
Recovery from liver resection varies, with most patients needing several weeks to a few months to fully recover. Initial recovery in the hospital involves managing pain, monitoring liver function, and gradually reintroducing liquids and foods. Patients are advised to avoid strenuous activities, heavy lifting, and alcohol consumption during the recovery period. Follow-up appointments are essential to monitor liver function, manage any complications, and assess the patient’s overall recovery.Estimated Cost
The cost of liver resection can vary based on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments, such as chemotherapy or radiation, are required. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for liver resection involves managing pain, preventing infection, and ensuring proper liver function. Patients are usually prescribed pain relievers and may be given antibiotics to prevent infection. Regular follow-up appointments are essential to monitor liver function, manage any complications, and adjust the treatment plan as needed. Nutritional support may be necessary, particularly if a large portion of the liver was removed. It is important to report any signs of complications, such as jaundice, severe pain, fever, or changes in appetite, promptly.

Pancreatectomy
- Purpose: Removes part or all of the pancreas to treat pancreatic cancer or pancreatitis.
- Procedure: The affected portion of the pancreas is surgically removed.
-
Note: The information provided here applies to routine Pancreatectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the extent of the surgery (partial or total pancreatectomy), the underlying condition being treated, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Pancreatectomy is typically performed as an inpatient procedure, requiring a hospital stay for close monitoring and initial recovery. The length of stay depends on the extent of the surgery and the patient’s overall condition.Hospital Stay Duration
Patients undergoing pancreatectomy usually stay in the hospital for 7 to 14 days, depending on the complexity of the surgery and the patient’s recovery progress. Longer stays may be necessary if complications arise or if additional treatments are required.Type of Anesthesia
Pancreatectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 4 to 6 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications, such as infection, bleeding, or diabetes management.Pre-procedure Preparation
Preparation for pancreatectomy involves following specific guidelines provided by the healthcare provider. This may include fasting before surgery, adjusting certain medications, and undergoing pre-operative tests such as blood work, imaging studies, and possibly an evaluation by an endocrinologist. A thorough evaluation by the surgical team is necessary to plan the surgery and manage any risks.Procedure Duration
The pancreatectomy procedure typically takes about 4 to 8 hours, depending on the extent of the surgery. A partial pancreatectomy involves removing part of the pancreas, while a total pancreatectomy involves removing the entire pancreas, along with the spleen, and possibly parts of other nearby organs. The surgery is complex and may also include the removal of surrounding lymph nodes.Recovery Time
Recovery from pancreatectomy varies, with most patients needing several weeks to a few months to fully recover. Initial recovery in the hospital involves managing pain, monitoring blood sugar levels, and gradually reintroducing liquids and foods. Patients may need to take enzyme supplements and insulin if the entire pancreas is removed. Strenuous activities, heavy lifting, and alcohol consumption should be avoided during the recovery period. Follow-up appointments are essential to monitor recovery, manage any complications, and adjust the treatment plan as needed.Estimated Cost
The cost of pancreatectomy can vary based on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments, such as chemotherapy or radiation, are required. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for pancreatectomy involves managing pain, preventing infection, and ensuring proper nutrition and blood sugar control. Patients will need regular follow-up appointments to monitor recovery and manage any complications, such as diabetes or digestive issues. Nutritional support, including enzyme supplements and a special diet, may be necessary, particularly if a large portion of the pancreas was removed. It is important to report any signs of complications, such as jaundice, severe pain, fever, or changes in appetite, promptly.
Adrenalectomy
- Purpose: Removes one or both adrenal glands to treat tumors or adrenal gland disorders.
- Procedure: The adrenal glands are surgically removed through an incision in the abdomen.
-
Note: The information provided here applies to routine Adrenalectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the underlying condition being treated (e.g., adrenal tumors, Cushing's syndrome, or pheochromocytoma), patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Adrenalectomy is typically performed as an inpatient procedure, requiring a hospital stay for close monitoring and initial recovery. The length of stay depends on the complexity of the surgery and the patient’s overall condition.Hospital Stay Duration
Patients undergoing adrenalectomy usually stay in the hospital for 2 to 5 days, depending on the complexity of the surgery and the patient’s recovery progress. Longer stays may be necessary if complications arise or if the patient requires more intensive post-operative care.Type of Anesthesia
Adrenalectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications, such as infection or hormonal imbalances.Pre-procedure Preparation
Preparation for adrenalectomy involves following specific guidelines provided by the healthcare provider. This may include fasting before surgery, adjusting certain medications, and undergoing pre-operative tests such as blood work, imaging studies, and possibly an evaluation by an endocrinologist. Patients with hormone-secreting tumors may need specific medical management to stabilize hormone levels before surgery.Procedure Duration
The adrenalectomy procedure typically takes about 2 to 4 hours, depending on whether a unilateral (one adrenal gland) or bilateral (both adrenal glands) adrenalectomy is being performed. The surgery can be done laparoscopically (minimally invasive) or through an open approach, depending on the size of the tumor and the surgeon’s assessment.Recovery Time
Recovery from adrenalectomy varies, with most patients needing several weeks to fully recover. Initial recovery in the hospital involves managing pain, monitoring hormone levels, and gradually reintroducing liquids and foods. Patients are advised to avoid strenuous activities, heavy lifting, and stress during the recovery period, as these can impact healing and hormone balance. Follow-up appointments are essential to monitor hormone levels, manage any complications, and adjust medication if needed.Estimated Cost
The cost of adrenalectomy can vary based on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments, such as medication for hormone management, are required. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for adrenalectomy involves managing pain, preventing infection, and ensuring proper hormone balance. Patients will need regular follow-up appointments to monitor recovery and manage any complications, such as adrenal insufficiency or imbalances in electrolytes. Hormone replacement therapy may be necessary if both adrenal glands are removed. It is important to report any signs of complications, such as fatigue, dizziness, or changes in blood pressure, promptly.
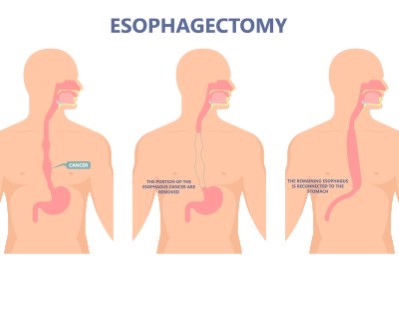
Esophagectomy
- Purpose: Removes part or all of the esophagus to treat esophageal cancer or severe damage.
- Procedure: The affected portion of the esophagus is surgically removed.
-
Note: The information provided here applies to routine Esophagectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the underlying reason for the surgery (e.g., esophageal cancer, Barrett's esophagus, or severe esophageal injury), patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Esophagectomy is typically performed as an inpatient procedure, requiring a hospital stay for close monitoring and initial recovery. Due to the complexity of the surgery, the patient’s hospital stay may be longer compared to other procedures.Hospital Stay Duration
Patients undergoing esophagectomy usually stay in the hospital for 7 to 14 days, depending on the complexity of the surgery, the patient’s recovery progress, and the management of any complications such as infection, anastomotic leaks, or respiratory issues.Type of Anesthesia
Esophagectomy is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 4 to 6 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications such as infection, difficulty swallowing, or nutritional issues.Pre-procedure Preparation
Preparation for esophagectomy involves following specific guidelines provided by the healthcare provider. This may include fasting before surgery, adjusting certain medications, and undergoing pre-operative tests such as blood work, imaging studies, and possibly an evaluation by a nutritionist or dietitian. Patients may also undergo pulmonary function tests and may need to stop smoking if applicable.Procedure Duration
The esophagectomy procedure typically takes 4 to 8 hours, depending on the extent of the surgery. During the surgery, part or all of the esophagus is removed, and the remaining portion is reconnected to the stomach or a portion of the intestine. The surgery can be performed using various techniques, including transthoracic, transhiatal, or minimally invasive approaches, depending on the patient's condition and the surgeon’s assessment.Recovery Time
Recovery from esophagectomy varies, with most patients needing several weeks to a few months to fully recover. Initial recovery in the hospital involves managing pain, monitoring for complications such as leaks or infections, and gradually reintroducing nutrition, often starting with a liquid diet. Patients may experience difficulty swallowing and changes in eating habits, requiring dietary adjustments and nutritional support. Strenuous activities and heavy lifting should be avoided during the recovery period. Follow-up appointments are essential to monitor recovery, manage any complications, and adjust the treatment plan as needed.Estimated Cost
The cost of esophagectomy can vary based on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments such as chemotherapy or radiation are required. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for esophagectomy involves managing pain, preventing infection, and ensuring proper nutrition and swallowing function. Patients will need regular follow-up appointments to monitor recovery, manage any complications, and address issues related to swallowing and nutrition. Nutritional support, including specialized diets and possibly feeding tubes, may be necessary during the initial recovery period. It is important to report any signs of complications, such as fever, difficulty swallowing, significant weight loss, or respiratory issues, promptly.
_20240719154442330182__0.webp)
Whipple Procedure (Pancreaticoduodenectomy)
- Purpose: Treats pancreatic cancer and other disorders by removing parts of the pancreas, small intestine, and gallbladder.
- Procedure: The head of the pancreas, part of the small intestine, and the gallbladder are surgically removed.
-
Note: The information provided here applies to routine Whipple Procedure (Pancreaticoduodenectomy) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the underlying reason for the surgery (e.g., pancreatic cancer, bile duct cancer, or chronic pancreatitis), patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
The Whipple Procedure is a major surgery that is always performed as an inpatient procedure. Due to its complexity, patients require a hospital stay for close monitoring and initial recovery.Hospital Stay Duration
Patients undergoing the Whipple Procedure usually stay in the hospital for 7 to 14 days, depending on the complexity of the surgery and the patient’s recovery progress. Longer stays may be necessary if complications arise, such as infection, anastomotic leaks, or delayed gastric emptying.Type of Anesthesia
The Whipple Procedure is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 4 to 6 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications, such as infection or issues with digestion.Pre-procedure Preparation
Preparation for the Whipple Procedure involves following specific guidelines provided by the healthcare provider. This may include fasting before surgery, adjusting certain medications, and undergoing pre-operative tests such as blood work, imaging studies, and possibly a nutritional assessment. Patients may also receive instructions on bowel preparation and managing any existing conditions such as diabetes.Procedure Duration
The Whipple Procedure typically takes 5 to 8 hours. During the surgery, the surgeon removes the head of the pancreas, part of the small intestine (duodenum), the gallbladder, and sometimes part of the stomach and bile duct. The remaining organs are then reconnected to allow digestion to continue. Due to the complexity of the procedure, it requires significant surgical expertise.Recovery Time
Recovery from the Whipple Procedure is extensive, with most patients needing several months to fully recover. Initial recovery in the hospital involves managing pain, monitoring for complications, and gradually reintroducing nutrition. Patients may experience changes in digestion, requiring dietary adjustments and possibly enzyme supplementation. Strenuous activities and heavy lifting should be avoided during the recovery period. Follow-up appointments are essential to monitor recovery, manage any complications, and adjust the treatment plan, including any additional cancer therapies if necessary.Estimated Cost
The cost of the Whipple Procedure can vary significantly based on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments, such as chemotherapy or radiation, are required. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for the Whipple Procedure involves managing pain, preventing infection, and ensuring proper nutrition and digestion. Patients will need regular follow-up appointments to monitor recovery, manage any complications, and address issues related to digestion and nutrition. Nutritional support, including a specialized diet and possibly enzyme supplements, may be necessary during the initial recovery period. It is important to report any signs of complications, such as fever, severe pain, jaundice, or significant weight loss, promptly.

Laparoscopic Surgery
- Purpose: Minimally invasive surgery to diagnose and treat various abdominal and pelvic conditions.
- Procedure: Small incisions are made, and a laparoscope is used to visualize and perform surgery.
-
Note: The information provided here applies to routine Laparoscopic Surgery procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the type of surgery being performed, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Laparoscopic surgery is often performed as an outpatient procedure, meaning most patients can return home the same day. However, depending on the complexity of the surgery and the patient’s overall health, an overnight stay may be required for observation.Hospital Stay Duration
For most laparoscopic surgeries, patients do not require an overnight hospital stay and can be discharged within a few hours after the procedure. If the surgery is more complex, or if complications arise, a short hospital stay of 1 to 2 days may be necessary.Type of Anesthesia
Laparoscopic surgery is typically performed under general anesthesia, meaning the patient will be fully unconscious during the procedure. In some cases, local anesthesia with sedation may be used, depending on the type of surgery and the patient’s needs.Travel After Procedure
Patients are generally able to travel shortly after the procedure, though it is advisable to rest for the remainder of the day. Long-distance travel should be avoided for at least 1 to 2 weeks, especially if the surgery was more complex, to allow time for initial recovery and monitoring for potential complications.Pre-procedure Preparation
Preparation for laparoscopic surgery involves following specific guidelines provided by the healthcare provider. Patients may be advised to fast before surgery, avoid certain medications, and undergo pre-operative tests such as blood work or imaging studies. Patients should also inform their surgical team of any existing medical conditions or medications they are taking.Procedure Duration
The duration of laparoscopic surgery varies depending on the type of surgery being performed. Most procedures take between 30 minutes to 2 hours. During the surgery, small incisions are made, and a camera (laparoscope) and specialized instruments are inserted to perform the procedure. This minimally invasive approach usually results in less pain and quicker recovery compared to open surgery.Recovery Time
Recovery from laparoscopic surgery is generally quicker than from open surgery. Most patients can resume light activities within a few days and return to normal activities within 1 to 2 weeks. However, recovery time can vary depending on the type of surgery performed and the patient’s overall health. Patients should avoid heavy lifting and strenuous activities for several weeks and follow their healthcare provider’s instructions for wound care and activity restrictions.Estimated Cost
The cost of laparoscopic surgery can vary depending on the type of surgery, the surgeon's expertise, and geographic location. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for laparoscopic surgery involves managing pain, preventing infection, and ensuring proper healing. Patients may be prescribed pain relievers and may be advised to avoid certain activities that could strain the surgical site. Follow-up appointments are typically scheduled to monitor recovery and remove any sutures if necessary. It is important to report any signs of complications, such as fever, severe pain, or unusual discharge from the incision sites, promptly.
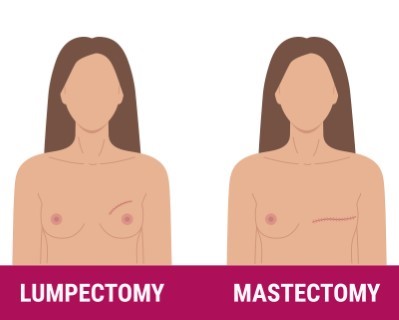
Breast Lumpectomy
- Purpose: Removes a breast lump or tumor while conserving breast tissue.
- Procedure: The lump or tumor is surgically removed, and surrounding tissue is examined.
-
Note: The information provided here applies to routine Breast Lumpectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the size and location of the tumor, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health and the complexity of the surgery can also influence the recovery process.
Inpatient/Outpatient
Breast lumpectomy is typically performed as an outpatient procedure, meaning most patients can return home the same day after a short observation period.Hospital Stay Duration
Patients undergoing a breast lumpectomy usually do not require an overnight hospital stay and can be discharged within a few hours after the procedure, once they are fully awake and stable.Type of Anesthesia
Breast lumpectomy is typically performed under local anesthesia with sedation or general anesthesia, depending on the patient’s preference and the surgeon’s recommendation. Local anesthesia with sedation keeps the patient relaxed and pain-free while awake, while general anesthesia ensures the patient is fully unconscious during the procedure.Travel After Procedure
Patients are generally advised to rest for the remainder of the day after the procedure and avoid strenuous activities. Long-distance travel is usually safe within a few days, but patients should follow specific recommendations from their healthcare provider regarding travel and activity levels.Pre-procedure Preparation
Preparation for breast lumpectomy involves following specific guidelines provided by the healthcare provider. Patients may be advised to fast before surgery, avoid certain medications, and undergo pre-operative tests such as blood work or imaging studies. It is important to inform the surgical team of any medications the patient is taking, particularly blood thinners, as these may need to be adjusted before surgery.Procedure Duration
The breast lumpectomy procedure typically takes about 1 to 2 hours, depending on the size and location of the tumor. During the surgery, the surgeon removes the tumor along with a small margin of surrounding healthy tissue to ensure complete removal. The goal of the procedure is to conserve as much of the breast as possible while effectively treating the cancer or other abnormal tissue.Recovery Time
Recovery from breast lumpectomy is generally quick, with most patients able to resume light activities within a few days and return to normal activities within 1 to 2 weeks. Patients may experience some pain, swelling, and bruising in the breast area, which can be managed with pain relievers and ice packs. It is important to avoid heavy lifting and strenuous activities during the initial recovery period and to follow the healthcare provider’s instructions for wound care and activity restrictions.Estimated Cost
The cost of breast lumpectomy can vary depending on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments such as radiation therapy are required. For accurate cost information, patients should contact their healthcare provider or surgical center directly.Post-procedure Care
Post-procedure care for breast lumpectomy involves managing pain, preventing infection, and ensuring proper healing. Patients may be prescribed pain relievers and may need to wear a supportive bra to minimize discomfort. Follow-up appointments are essential to monitor recovery, discuss pathology results, and determine if further treatment, such as radiation or chemotherapy, is necessary. It is important to report any signs of complications, such as fever, severe pain, or unusual discharge from the incision site, promptly.
Parathyroidectomy
- Purpose: Removes one or more parathyroid glands to treat hyperparathyroidism.
- Procedure: The affected parathyroid glands are surgically removed.
-
Note: The information provided here applies to routine Parathyroidectomy procedures under typical conditions. However, specifics may vary depending on individual patient factors, such as the number of glands affected, underlying health conditions, or any complications that might arise during or after the surgery. The patient’s overall health and the complexity of the procedure can also affect the recovery process.
Inpatient/Outpatient
Parathyroidectomy is usually performed as an outpatient procedure, allowing most patients to return home the same day after a brief observation period. However, in some cases, particularly if complications occur, an overnight stay may be required.Hospital Stay Duration
For most parathyroidectomies, patients are discharged a few hours after the procedure, once they have fully recovered from anesthesia and are stable. An overnight stay may be necessary if there are concerns about calcium levels or other post-operative issues.Type of Anesthesia
Parathyroidectomy is generally performed under general anesthesia, ensuring that the patient is fully unconscious during the surgery. In some instances, local anesthesia with sedation may be an option, depending on the patient’s condition and the surgeon’s preference.Travel After Procedure
Patients are usually advised to rest for the remainder of the day following the procedure and to avoid strenuous activities for a short period. Traveling is generally safe within a few days, but it’s important to follow the specific recommendations provided by the healthcare team.Pre-procedure Preparation
Preparation for parathyroidectomy involves adhering to specific guidelines provided by the healthcare provider. Patients may be instructed to fast before the surgery, avoid certain medications, and undergo pre-operative tests such as blood work and imaging studies. It is important to disclose any medications the patient is taking, especially those that could affect blood clotting.Procedure Duration
The parathyroidectomy procedure typically lasts between 1 to 2 hours, depending on the number of glands that need to be removed and the complexity of the surgery. The surgeon removes the overactive or diseased parathyroid glands through a small incision in the neck. The goal is to restore normal calcium levels in the blood while preserving as much healthy tissue as possible.Recovery Time
Recovery from parathyroidectomy is usually swift, with many patients able to resume light activities within a few days and return to normal activities within 1 to 2 weeks. Some swelling, mild pain, and discomfort in the neck area are common after the surgery and can be managed with pain medications and proper wound care. Patients should avoid heavy lifting and strenuous activities during the initial recovery phase.Estimated Cost
The cost of parathyroidectomy can vary based on the surgeon's experience, the complexity of the procedure, the geographic location, and whether additional treatments are needed. For precise cost details, patients should consult their healthcare provider or surgical facility directly.Post-procedure Care
Post-procedure care for parathyroidectomy involves managing pain, monitoring calcium levels, and ensuring proper healing. Patients may need to take calcium and vitamin D supplements to maintain normal levels and prevent hypocalcemia, a common temporary condition after surgery. Follow-up appointments are crucial to check calcium levels, assess recovery, and address any concerns. It is important to report any symptoms of low calcium, such as tingling, muscle cramps, or confusion, to the healthcare provider immediately.
Bowel Resection
- Purpose: Removes part of the bowel to treat cancer, blockages, or other bowel diseases.
- Procedure: The affected section of the bowel is surgically removed.
-
Note: The information provided here applies to routine Bowel Resection procedures under typical conditions. However, specifics may vary depending on individual patient factors, such as the underlying condition (e.g., cancer, Crohn’s disease, or diverticulitis), the extent of the resection, and any complications that might arise during or after surgery. The patient’s overall health and the complexity of the procedure can also impact the recovery process.
Inpatient/Outpatient
Bowel resection is typically performed as an inpatient procedure, requiring a hospital stay for close monitoring and initial recovery. The duration of the hospital stay depends on the extent of the surgery and the patient's overall condition.Hospital Stay Duration
Patients undergoing bowel resection generally stay in the hospital for 5 to 7 days, depending on the complexity of the surgery and how well they are recovering. A longer stay may be necessary if complications arise, such as infection, bowel obstruction, or difficulty resuming normal bowel function.Type of Anesthesia
Bowel resection is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. This ensures that the patient is comfortable and pain-free throughout the procedure.Travel After Procedure
Patients are usually advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after the procedure. This allows time for initial recovery and monitoring for potential complications, such as infection or issues with bowel function.Pre-procedure Preparation
Preparation for bowel resection typically involves following specific guidelines provided by the healthcare provider. This may include fasting before surgery, bowel preparation to cleanse the intestines, and possibly adjusting medications, particularly blood thinners. Pre-operative tests, such as blood work, imaging studies, and possibly a colonoscopy, may be required to plan the surgery.Procedure Duration
The duration of the bowel resection procedure varies depending on the extent of the surgery. It typically takes between 2 to 4 hours. During the surgery, the surgeon removes the diseased or damaged portion of the bowel and reconnects the healthy sections. In some cases, a temporary or permanent stoma (an opening in the abdomen for waste elimination) may be necessary.Recovery Time
Recovery from bowel resection can take several weeks to a few months, depending on the complexity of the surgery and the patient’s overall health. Initially, patients will be closely monitored in the hospital, where they will gradually reintroduce liquids and foods and manage pain. Once discharged, patients should avoid strenuous activities, heavy lifting, and high-fiber or difficult-to-digest foods until they have fully healed. Follow-up appointments are essential to monitor healing, assess bowel function, and manage any complications.Estimated Cost
The cost of bowel resection can vary depending on the surgeon's expertise, the complexity of the procedure, geographic location, and whether additional treatments, such as chemotherapy or radiation, are needed. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for bowel resection involves managing pain, monitoring bowel function, and ensuring proper healing. Patients may be prescribed pain relievers and antibiotics to prevent infection. It is important to follow dietary recommendations, starting with soft, easy-to-digest foods and gradually reintroducing regular meals. Patients with a stoma will receive instructions on stoma care and management. Any signs of complications, such as fever, severe pain, changes in bowel habits, or issues with the stoma, should be reported to the healthcare provider immediately.

Appendectomy
- Purpose: Removes the appendix to treat appendicitis.
- Procedure: The appendix is surgically removed through an incision in the abdomen.
-
Note: The information provided here pertains to standard Appendectomy procedures under typical circumstances. However, details may vary depending on individual patient factors, such as the severity of appendicitis, patient response, or any complications that might arise during or after the operation. The patient’s overall health and the complexity of the surgery can also impact the recovery process.
Inpatient/Outpatient
Appendectomy is often performed as an inpatient procedure, especially if complications such as perforation or abscess formation are present. This allows for close monitoring and management of any post-operative issues. Even in uncomplicated cases, patients might be kept overnight for observation.Hospital Stay Duration
For uncomplicated appendicitis, patients typically remain in the hospital for 1 to 2 days to ensure stable recovery and effective pain management. If the appendix has ruptured or if there are complications, a hospital stay of 3 to 5 days or longer may be necessary to manage infection and ensure a safe recovery.Type of Anesthesia
Appendectomy is conducted under general anesthesia, ensuring the patient is fully asleep and pain-free during the surgery. This approach is standard for providing patient comfort and ensuring the procedure can be performed effectively.Travel After Procedure
Patients are generally advised to refrain from travel, especially long-distance or air travel, for at least 2 to 4 weeks after surgery. This precaution allows time for initial healing and monitoring for any potential complications, such as infection or wound issues.Pre-procedure Preparation
Preparation for appendectomy is typically minimal due to the emergency nature of most cases. Patients may be asked to avoid eating or drinking for several hours before the operation, and pre-operative tests like blood work and imaging studies may be done to confirm the diagnosis.Procedure Duration
The appendectomy procedure typically lasts about 30 minutes to 1 hour. During the surgery, the surgeon removes the inflamed or infected appendix. This can be performed using a laparoscopic (minimally invasive) approach, which involves small incisions and specialized tools, or through an open approach with a larger incision, depending on the condition’s severity and the patient’s specific circumstances.Recovery Time
Recovery from appendectomy is generally swift, with most patients able to return to light activities within a few days and resume normal routines within 1 to 2 weeks. Patients may experience some discomfort or pain at the incision site, which can be managed with prescribed pain relief. It’s important to avoid heavy lifting and strenuous activities during the initial recovery phase to prevent complications.Estimated Cost
The cost of appendectomy can vary based on the surgeon's experience, the complexity of the surgery (laparoscopic vs. open), geographic location, and whether complications necessitate additional care. For precise cost information, patients should consult their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care after an appendectomy involves managing pain, preventing infection, and ensuring proper healing. Patients should adhere to their healthcare provider’s instructions on caring for the surgical site, including keeping the area clean and dry. Antibiotics may be prescribed if the appendix was perforated or if there was significant infection. Follow-up appointments are typically scheduled to monitor recovery and address any concerns. It is important to promptly report any signs of complications, such as fever, increased pain, or unusual discharge from the incision site.