Cardiology Treatments

Coronary Angiography
- Purpose: Diagnoses coronary artery disease by visualizing blood flow in the coronary arteries.
- Procedure: A catheter is inserted through the groin or arm and guided to the coronary arteries, where a contrast dye is injected for X-ray imaging.
Note: The information provided here applies to elective situations and assumes there are no extraordinary circumstances or the need for additional interventions. Please note that these details can vary for each patient depending on factors such as proceeding coronary interventions, complications, or other situations like patient-specific health conditions, unexpected findings during the procedure, or individual recovery rates.
Inpatient/Outpatient
Coronary angiography is typically performed as an outpatient procedure. This means that most patients can go home on the same day as the procedure, barring any complications or the need for further interventions.
Hospital Stay Duration
Most patients are monitored for a few hours after the procedure and are usually discharged on the same day. In rare cases, an overnight stay may be required.
Type of Anesthesia
The procedure is usually performed under local anesthesia, with the option of sedation if needed to keep the patient comfortable during the procedure.
Travel After Procedure
Patients are generally advised that they can travel the same day or the day after the procedure, depending on their recovery and the advice of their healthcare provider.
Pre-procedure Preparation
Patients are typically asked to fast for 4-6 hours before the procedure. They may also need to adjust their medications according to their doctor's instructions.
Procedure Duration
The procedure usually takes between 30 minutes to 1 hour to complete.
Recovery Time
Most patients can return to normal activities within a few hours after the procedure, though rest is recommended for the remainder of the day.
Estimated Cost
The cost of coronary angiography can vary depending on the hospital and country. For more detailed information on costs, please contact us directly.
Post-procedure Care
Post-procedure care involves monitoring the catheter insertion site for any signs of bleeding or infection. Patients are advised to avoid strenuous activities for a few days after the procedure.
-_-coronary-angioplasty_20240716165210982043__0.webp)
Percutaneous Coronary Intervention (PCI) / Coronary Angioplasty
- Purpose: Treats narrowed or obstructed coronary arteries by restoring blood flow.
- Procedure: During PCI, a catheter with a small balloon at its tip is inserted through an artery in the groin or arm and guided to the narrowed section of the coronary artery. Once positioned, the balloon is inflated to compress the plaque against the artery walls, widening the artery to improve blood flow. In most cases, a stent—a small mesh tube—is then placed at the site of the blockage to keep the artery open long-term.
-
Note: The information provided here applies to elective PCI procedures without extraordinary circumstances. However, the specifics may vary based on individual patient factors, such as the presence of multiple blockages, underlying heart conditions, or complications that may arise during the procedure. In some cases, the procedure may be more complex, requiring additional interventions or extended hospital stays.
Inpatient/Outpatient
PCI is typically performed as an inpatient procedure, particularly in cases where multiple arteries are treated, the patient has other underlying health conditions, or the risk of complications is higher. Patients may need to stay in the hospital for monitoring after the procedure, especially if it is part of an emergency treatment or if complications arise during the intervention.Hospital Stay Duration
Most patients undergoing PCI are monitored for several hours post-procedure. Depending on the complexity of the procedure and the patient's overall condition, a hospital stay of one or more nights may be required to ensure a safe recovery and to monitor for any potential complications.Type of Anesthesia
Local anesthesia is used to numb the area where the catheter is inserted, typically in the groin or arm. Mild sedation is often administered to keep the patient comfortable during the procedure. In certain cases, such as with patients who may not tolerate the procedure well, general anesthesia may be considered.Travel After Procedure
Travel is generally not recommended for at least 24 hours after PCI, particularly if sedation was used. Patients are advised to consult with their healthcare provider before planning any travel, especially long-distance or air travel, to ensure they are fit for travel and that there are no immediate post-procedure complications.Pre-procedure Preparation
Patients are usually required to fast for several hours before the procedure. They may also need to temporarily stop certain medications, especially blood thinners, under the guidance of their healthcare provider to minimize the risk of bleeding during the procedure.Procedure Duration
The PCI procedure typically takes 1 to 2 hours, although this can vary depending on the number of blockages being treated and the complexity of the case.Recovery Time
Recovery time varies, but most patients can resume light activities within a few days. Full recovery, including returning to normal physical activity, generally takes about a week, though this may vary depending on the patient’s overall health and the specifics of their treatment.Estimated Cost
The cost of PCI can vary depending on the hospital, geographic location, and the specific details of the procedure, such as the number of stents placed. For more detailed cost information, patients should contact their healthcare provider directly.Post-procedure Care
Post-procedure care includes monitoring the insertion site for signs of infection, swelling, or bleeding. Patients will also be prescribed antiplatelet medications to prevent blood clots in the stent and should follow up with their healthcare provider for further instructions on lifestyle modifications, medication management, and future appointments.
_20240716165317590784__0.webp)
Electrophysiology Study (EPS)
- Purpose: Diagnoses and treats abnormal heart rhythms.
- Procedure: Catheters with electrodes are inserted into the heart to map its electrical activity.
-
Note: The information provided here applies to elective Electrophysiology Studies (EPS) without extraordinary circumstances. However, the specifics may vary depending on individual patient factors, such as the complexity of the heart rhythm disorder being investigated, underlying heart conditions, or any complications that might arise during the procedure. In some cases, additional interventions like catheter ablation might be performed during the same session.
Inpatient/Outpatient
EPS is often performed as an inpatient procedure, especially when there is a higher risk of complications or when additional procedures, such as catheter ablation, are planned to treat the detected arrhythmias. Patients may need to stay in the hospital for observation after the study to ensure their heart rhythm remains stable.Hospital Stay Duration
Most patients undergoing EPS are monitored for several hours after the procedure. Depending on the findings and whether additional interventions are performed, a hospital stay of one night or more may be required to monitor heart rhythm stability and manage any immediate post-procedure effects.Type of Anesthesia
EPS is typically performed under local anesthesia at the catheter insertion sites, with mild sedation provided to keep the patient comfortable. In some cases, general anesthesia may be used, particularly if the patient requires additional interventions during the procedure or if the patient’s condition necessitates it.Travel After Procedure
Patients are usually advised to avoid travel for at least 24 hours after EPS, particularly if sedation was used. Depending on the patient’s recovery and whether any additional treatments were performed, longer travel, including flights, may be postponed for a few days.Pre-procedure Preparation
Patients are generally instructed to fast for several hours before EPS. They may also need to temporarily stop certain medications, particularly those that affect heart rhythm, as directed by their healthcare provider to ensure accurate test results.Procedure Duration
The duration of an EPS can vary, typically lasting between 1 to 4 hours depending on the complexity of the heart rhythm disorder being studied and whether any additional procedures, like catheter ablation, are performed.Recovery Time
Most patients can resume light activities within a day or two after EPS, although full recovery may take a few days depending on the patient’s overall condition and the extent of the procedure. Patients should follow their healthcare provider’s recommendations regarding activity levels post-procedure.Estimated Cost
The cost of EPS can vary depending on the hospital, geographic location, and whether additional treatments, such as catheter ablation, are required during the procedure. For specific pricing details, patients should contact their healthcare provider.Post-procedure Care
Post-procedure care includes monitoring the catheter insertion sites for any signs of bleeding, swelling, or infection. Patients will also need to follow up with their healthcare provider to discuss the results of the study and any necessary changes to their treatment plan, including medications or further procedures.

Radiofrequency Catheter Ablation
- Purpose: Treats abnormal heart rhythms by destroying the area of heart tissue causing the arrhythmia.
- Procedure: Similar to EPS, but involves delivering radiofrequency energy to ablate the problematic tissue.
-
Note: The information provided here applies to elective Radiofrequency Catheter Ablation procedures without extraordinary circumstances. However, the specifics may vary based on individual patient factors, such as the type and complexity of the arrhythmia being treated, underlying heart conditions, or any complications that may arise during the procedure. Additional factors, such as the need for multiple ablations or extended monitoring, can also affect the treatment plan.
Inpatient/Outpatient
Radiofrequency Catheter Ablation is typically performed as an inpatient procedure, especially when treating complex arrhythmias or when the patient has other underlying heart conditions that require closer monitoring. Patients may be admitted for observation after the procedure to ensure the arrhythmia has been effectively treated and that no complications arise.Hospital Stay Duration
Patients usually stay in the hospital for at least one night following the procedure. This allows for continuous monitoring of the heart’s rhythm and ensures that any immediate post-procedure complications, such as bleeding or recurrence of arrhythmia, are managed promptly.Type of Anesthesia
The procedure is usually performed under local anesthesia at the catheter insertion site, combined with mild sedation to keep the patient comfortable. In some cases, general anesthesia may be used, particularly if the procedure is expected to be lengthy or if the patient’s condition warrants it.Travel After Procedure
Patients are generally advised to avoid travel for at least 24 to 48 hours after the procedure, depending on their recovery and any post-procedure instructions from their healthcare provider. Longer or more strenuous travel may be postponed for several days to ensure the patient is fully stable.Pre-procedure Preparation
Before the procedure, patients are typically asked to fast for several hours. They may also need to stop taking certain medications, particularly those affecting heart rhythm, as instructed by their healthcare provider to optimize the success of the ablation.Procedure Duration
The procedure usually lasts between 2 to 4 hours, depending on the complexity of the arrhythmia being treated and the number of areas in the heart that require ablation.Recovery Time
Most patients can return to light activities within a few days, though full recovery and a return to normal activity levels may take about a week. It’s important to follow the healthcare provider’s recommendations on activity restrictions post-procedure.Estimated Cost
The cost of Radiofrequency Catheter Ablation can vary depending on the hospital, geographic location, and the specifics of the procedure. Factors such as the duration of the procedure and the complexity of the arrhythmia can also affect the cost. For precise pricing information, patients should contact their healthcare provider.Post-procedure Care
After the procedure, patients need to monitor the catheter insertion site for signs of infection, bleeding, or swelling. Regular follow-up appointments with a healthcare provider are crucial to assess the success of the ablation and to manage any ongoing care, such as adjustments to medications or further treatments if necessary.
_20240719162432222845__0.webp)
Transesophageal Echocardiography (TEE)
- Purpose: Provides detailed images of the heart's structure and function, often used when more detailed imaging is required than standard echocardiography can provide.
- Procedure: A probe is inserted into the esophagus, which is located close to the heart, to obtain high-resolution images using ultrasound.
-
Note: The information provided here applies to elective Transesophageal Echocardiography (TEE) procedures without extraordinary circumstances. However, the specifics may vary depending on individual patient factors, such as the presence of other heart conditions, patient tolerance to the procedure, or complications that might arise during or after the procedure. Additionally, TEE is often performed in conjunction with other diagnostic or therapeutic interventions, which could affect the procedure's complexity and duration.
Inpatient/Outpatient
TEE is typically performed as an outpatient procedure, but in some cases, it may be done in an inpatient setting, especially if the patient is already hospitalized for other reasons or if TEE is part of a more comprehensive evaluation or treatment plan. If complications are expected or if the patient has significant comorbidities, they may be monitored in the hospital for a short period post-procedure.Hospital Stay Duration
Most patients can expect to go home the same day after TEE, typically within a few hours of the procedure. However, if TEE is conducted alongside other procedures or if the patient experiences complications such as persistent throat discomfort or arrhythmias, an overnight stay might be required for further observation.Type of Anesthesia
The procedure is usually performed under conscious sedation, combined with a local anesthetic spray to numb the throat. This helps to minimize discomfort while the probe is inserted into the esophagus. In some cases, general anesthesia might be used, particularly if the patient cannot tolerate sedation or if TEE is performed in conjunction with other more invasive procedures.Travel After Procedure
Patients are generally advised to avoid travel for at least 24 hours after the procedure, particularly if sedation was used. This allows time for the sedation to wear off completely and for any minor discomfort from the procedure to subside.Pre-procedure Preparation
Patients are typically asked to fast for 4-6 hours before the procedure to ensure an empty stomach, which helps reduce the risk of aspiration during the procedure. Patients should also inform their healthcare provider of any medications they are taking, especially blood thinners, as adjustments may be necessary.Procedure Duration
TEE usually takes about 30 to 60 minutes to complete, though the total time spent at the medical facility may be longer due to pre-procedure preparation and post-procedure recovery.Recovery Time
Most patients recover quickly and can resume normal activities the day after the procedure. However, it is recommended to rest for the remainder of the day following the procedure, especially if sedation was used. Mild throat discomfort may persist for a day or two.Estimated Cost
The cost of TEE can vary depending on the hospital, geographic location, and whether the procedure is performed alongside other diagnostic tests or treatments. Patients should contact their healthcare provider or hospital for detailed pricing information.Post-procedure Care
After the procedure, patients may experience mild throat irritation or discomfort, which typically resolves within a day or two. Patients should follow up with their healthcare provider to review the results of the TEE and discuss any further diagnostic tests or treatments if necessary.

Pacemaker Insertion
- Purpose: Treats slow heart rhythms by providing electrical stimulation to maintain an adequate heart rate.
- Procedure: A device is implanted under the skin, with leads placed in the heart.
-
Note: The information provided here applies to elective Pacemaker Insertion procedures without extraordinary circumstances. However, the specifics may vary based on individual patient factors, such as the underlying heart condition necessitating the pacemaker, the type of pacemaker being implanted, and any complications that might arise during the procedure. In some cases, the patient's overall health, the presence of other medical conditions, or the need for additional cardiac interventions could also influence the procedure.
Inpatient/Outpatient
Pacemaker insertion is typically performed as an inpatient procedure. This allows for close monitoring of the patient before, during, and after the procedure to ensure that the pacemaker is functioning properly and that the patient's heart rhythm is stable. Most patients will require at least one night in the hospital for observation.Hospital Stay Duration
Patients undergoing pacemaker insertion usually stay in the hospital for 1 to 2 days. This allows for monitoring of the pacemaker's function, ensuring there are no immediate complications such as infection, bleeding, or lead displacement. Some patients with complex medical histories or who undergo additional procedures may require a longer hospital stay.Type of Anesthesia
The procedure is generally performed under local anesthesia at the site where the pacemaker is implanted, usually in the upper chest. Mild sedation is also provided to help the patient relax. General anesthesia is rarely used but may be considered in specific cases where the patient’s condition or the complexity of the procedure requires it.Travel After Procedure
Patients are typically advised to avoid travel for at least a few days after pacemaker insertion, particularly air travel, to allow time for initial recovery and to ensure the pacemaker is functioning properly. It’s important to follow the healthcare provider’s specific recommendations regarding travel and activity restrictions post-procedure.Pre-procedure Preparation
Before the procedure, patients are usually instructed to fast for several hours. They may also need to stop taking certain medications, particularly blood thinners, to reduce the risk of bleeding during the procedure. Patients should follow their healthcare provider's instructions closely to prepare for the procedure.Procedure Duration
The pacemaker insertion procedure typically takes about 1 to 2 hours, although this can vary depending on the complexity of the case and whether any additional procedures are performed at the same time.Recovery Time
Most patients can expect to return to light activities within a week, though full recovery, including a return to more strenuous activities, may take several weeks. It’s important to avoid heavy lifting or strenuous arm movements on the side where the pacemaker was implanted during the initial recovery period.Estimated Cost
The cost of pacemaker insertion can vary widely depending on the hospital, geographic location, and the type of pacemaker being implanted. Patients should contact their healthcare provider or hospital directly to obtain detailed cost information.Post-procedure Care
Post-procedure care involves monitoring the incision site for signs of infection, managing any discomfort with prescribed medications, and attending follow-up appointments to ensure the pacemaker is functioning correctly. Patients will also receive instructions on how to care for the incision site and any activity restrictions. Regular check-ups will be necessary to monitor the pacemaker’s performance and to adjust settings as needed.
-insertion_20240716170641908815__0.webp)
Implantable Cardioverter Defibrillator (ICD) Insertion
- Purpose: Prevents sudden cardiac death by detecting and treating life-threatening arrhythmias.
- Procedure: A device is implanted under the skin, with leads placed in the heart to monitor and correct abnormal rhythms.
-
Note: The information provided here applies to elective Implantable Cardioverter Defibrillator (ICD) insertion procedures without extraordinary circumstances. However, specifics may vary based on individual patient factors, such as the severity of the underlying heart condition, the type of ICD being implanted, and any complications that might arise during the procedure. In some cases, additional interventions, the patient’s overall health, or the presence of other medical conditions could also influence the procedure and recovery process.
Inpatient/Outpatient
ICD insertion is typically performed as an inpatient procedure. This allows for close monitoring before, during, and after the procedure to ensure that the device is functioning correctly and that the patient's heart rhythm is stable. Most patients will require at least one night in the hospital for observation and device testing.Hospital Stay Duration
Patients undergoing ICD insertion usually stay in the hospital for 1 to 2 days. This hospital stay ensures that the ICD is working properly and that there are no immediate complications such as lead displacement, infection, or arrhythmias. Patients with complex conditions or who require additional procedures may need a longer hospital stay.Type of Anesthesia
The procedure is typically performed under local anesthesia at the site where the ICD is implanted, usually in the upper chest. Mild sedation is also administered to help the patient relax during the procedure. General anesthesia may be used in specific cases, especially if the patient’s condition or the complexity of the procedure necessitates it.Travel After Procedure
Patients are generally advised to avoid travel for at least a few days after ICD insertion, particularly long-distance or air travel, to allow for initial recovery and to ensure the device is functioning correctly. It's important to follow the healthcare provider’s specific recommendations regarding travel and physical activity post-procedure.Pre-procedure Preparation
Prior to the procedure, patients are usually instructed to fast for several hours. They may also need to stop taking certain medications, especially blood thinners, to minimize the risk of bleeding during the procedure. Detailed instructions will be provided by the healthcare team to ensure the patient is adequately prepared.Procedure Duration
The ICD insertion procedure typically takes between 1 to 2 hours, though this can vary depending on the complexity of the case and whether additional procedures are required at the same time.Recovery Time
Most patients can return to light activities within a week, though full recovery and a return to more strenuous activities may take several weeks. During the initial recovery period, patients should avoid heavy lifting and strenuous arm movements on the side where the ICD was implanted to allow for proper healing.Estimated Cost
The cost of ICD insertion can vary depending on the hospital, geographic location, and the type of device being implanted. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
After the procedure, post-procedure care includes monitoring the incision site for signs of infection, managing discomfort with prescribed medications, and attending follow-up appointments to ensure the ICD is functioning correctly. Patients will receive detailed instructions on caring for the incision site, activity restrictions, and what to expect from the device. Regular follow-up visits are crucial to monitor the ICD’s performance and make any necessary adjustments to the device settings.
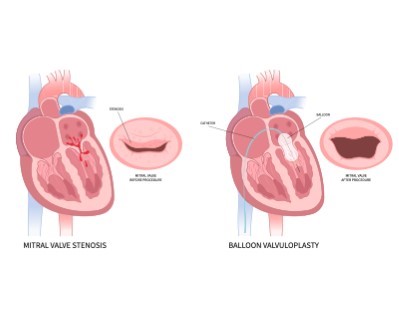
Mitral Balloon Valvuloplasty
- Purpose: Treats mitral valve stenosis by widening the mitral valve opening.
- Procedure: A balloon catheter is inserted into the mitral valve and inflated to stretch the valve.
-
Note: The information provided here applies to elective Mitral Balloon Valvuloplasty procedures without extraordinary circumstances. However, specifics may vary based on individual patient factors, such as the severity of mitral valve stenosis, the presence of other heart conditions, or complications that might arise during the procedure. In some cases, additional interventions or the patient’s overall health could influence the procedure and recovery process.
Inpatient/Outpatient
Mitral Balloon Valvuloplasty is typically performed as an inpatient procedure. This approach allows for close monitoring of the patient before, during, and after the procedure to ensure that the mitral valve is properly opened and that the patient's heart function remains stable. Most patients will require at least one night in the hospital for observation and recovery.Hospital Stay Duration
Patients undergoing Mitral Balloon Valvuloplasty usually stay in the hospital for 1 to 2 days. This hospital stay ensures that the procedure was successful and that there are no immediate complications, such as valve regurgitation, bleeding, or arrhythmias. Patients with more complex conditions may require a longer stay for additional monitoring.Type of Anesthesia
The procedure is generally performed under local anesthesia with sedation, which helps the patient remain comfortable and relaxed during the procedure. In some cases, general anesthesia may be used, especially if the patient has other medical conditions that make sedation alone insufficient or if the procedure is expected to be more complex.Travel After Procedure
Patients are typically advised to avoid travel for at least a few days after the procedure, particularly long-distance or air travel, to ensure that they are stable and to allow time for any immediate recovery needs. It’s important to follow the healthcare provider’s specific recommendations regarding travel and activity post-procedure.Pre-procedure Preparation
Prior to the procedure, patients are usually instructed to fast for several hours. They may also need to temporarily adjust or stop taking certain medications, especially blood thinners, under the guidance of their healthcare provider to minimize the risk of bleeding during the procedure. Specific pre-procedure tests and imaging may also be required to plan the procedure effectively.Procedure Duration
Mitral Balloon Valvuloplasty typically takes about 1 to 2 hours to complete, although the total time may vary depending on the complexity of the stenosis and the patient’s overall condition.Recovery Time
Most patients can expect to return to light activities within a week, though full recovery, including the resumption of more strenuous activities, may take several weeks. Patients should follow their healthcare provider’s instructions regarding activity levels and any necessary lifestyle adjustments post-procedure.Estimated Cost
The cost of Mitral Balloon Valvuloplasty can vary widely depending on the hospital, geographic location, and the specifics of the patient’s condition. For detailed cost information, patients should contact their healthcare provider or the hospital directly.Post-procedure Care
Post-procedure care involves monitoring the patient for signs of complications, such as valve leakage or arrhythmias. Patients will also need to manage the incision site (if applicable) and attend follow-up appointments to assess the success of the procedure and discuss any further treatment or lifestyle changes. Regular follow-ups are essential to monitor heart function and ensure the long-term success of the procedure.
_20240716231639652392__0.webp)
Transcatheter Aortic Valve Replacement (TAVR or TAVI)
- Purpose: Treats severe aortic stenosis by replacing the aortic valve without open-heart surgery.
- Procedure: A new valve is delivered via catheter and expanded within the existing valve.
Note: The information provided here applies to elective Transcatheter Aortic Valve Replacement (TAVR or TAVI) procedures without extraordinary circumstances. However, specifics may vary based on individual patient factors, such as the severity of aortic stenosis, the presence of other heart conditions, or any complications that might arise during the procedure. In some cases, the patient's overall health, the need for additional cardiac interventions, or the complexity of the valve replacement can also influence the procedure and recovery process.
Inpatient/Outpatient
TAVR is typically performed as an inpatient procedure. This approach allows for careful monitoring before, during, and after the procedure to ensure the new valve is functioning correctly and that the patient's heart condition is stable. Most patients will need to stay in the hospital for observation, typically for a few days, depending on their recovery and overall health.Hospital Stay Duration
Patients undergoing TAVR usually stay in the hospital for 2 to 5 days. This stay allows for close monitoring of heart function and valve performance, as well as the management of any potential complications such as bleeding, stroke, or arrhythmias. In some cases, the hospital stay may be extended if additional care or monitoring is needed.Type of Anesthesia
TAVR is typically performed under general anesthesia to ensure the patient remains comfortable and still during the procedure. In some cases, conscious sedation may be used, depending on the patient's condition and the preferences of the medical team.Travel After Procedure
Patients are generally advised to avoid travel for at least a week after the procedure, especially if they underwent general anesthesia or experienced any complications. It’s crucial to follow the healthcare provider’s recommendations regarding travel and to ensure that the patient is stable before undertaking any long-distance or air travel.Pre-procedure Preparation
Before the procedure, patients are usually instructed to fast for several hours. They may also need to undergo a series of tests, including imaging studies and blood work, to ensure they are good candidates for TAVR. Adjustments to medications, especially blood thinners, may also be required under the guidance of the healthcare provider.Procedure Duration
The TAVR procedure typically takes 1 to 2 hours to complete, though this can vary depending on the complexity of the case and the patient's specific condition.Recovery Time
Most patients can begin to resume light activities within a week of the procedure, though full recovery may take several weeks. It's important to avoid strenuous activities during this period and to follow the healthcare provider’s instructions regarding activity levels and any necessary lifestyle changes.Estimated Cost
The cost of TAVR can vary significantly depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
After TAVR, post-procedure care includes close monitoring of the new valve and overall heart function, managing any discomfort, and observing for potential complications. Patients will need to attend follow-up appointments to ensure the valve is working properly and to discuss any further treatment or lifestyle adjustments. Long-term follow-up is crucial to monitor the patient's heart health and the performance of the valve.
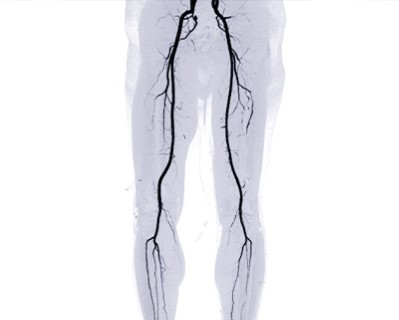
Peripheral Angiography
- Purpose: Diagnoses peripheral artery disease by visualizing blood flow in the peripheral arteries.
- Procedure: Similar to coronary angiography, but focuses on arteries outside the heart, such as in the legs.
-
Note: The information provided here applies to elective Peripheral Angiography procedures without extraordinary circumstances. However, specifics may vary based on individual patient factors, such as the extent of peripheral artery disease, the presence of other vascular conditions, or complications that might arise during the procedure. The patient’s overall health, the need for additional interventions, or the complexity of the angiography can also influence the procedure and recovery process.
Inpatient/Outpatient
Peripheral Angiography is typically performed as an outpatient procedure, allowing most patients to return home the same day. However, if the procedure reveals significant blockages that require immediate intervention, or if complications arise, a hospital stay might be necessary for further treatment and observation.Hospital Stay Duration
Most patients undergoing Peripheral Angiography are monitored for a few hours after the procedure and can usually be discharged on the same day. If additional treatments, such as angioplasty or stent placement, are performed during the same session, an overnight stay might be required to ensure the patient’s condition remains stable.Type of Anesthesia
The procedure is usually performed under local anesthesia at the catheter insertion site, often in the groin or arm. Mild sedation may also be administered to help the patient relax during the procedure. General anesthesia is rarely used but may be considered in specific cases depending on the patient’s condition.Travel After Procedure
Patients are generally advised to avoid travel for at least 24 hours after Peripheral Angiography, particularly if sedation was used. Depending on the findings and any additional procedures performed, longer or more strenuous travel may be postponed for a few days to ensure the patient is stable and comfortable.Pre-procedure Preparation
Before the procedure, patients are typically instructed to fast for several hours. They may also need to temporarily stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to reduce the risk of bleeding during the procedure.Procedure Duration
Peripheral Angiography usually takes about 1 to 2 hours, depending on the extent of the vascular examination and whether any additional interventions are performed during the procedure.Recovery Time
Most patients can resume light activities within a day or two after the procedure. However, it is recommended to avoid strenuous activities for several days, particularly those that could put stress on the catheter insertion site.Estimated Cost
The cost of Peripheral Angiography can vary depending on the hospital, geographic location, and whether any additional procedures, such as angioplasty or stenting, are performed. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care involves monitoring the catheter insertion site for signs of infection, bleeding, or swelling. Patients will also need to follow up with their healthcare provider to review the results of the angiography and discuss any further treatment or lifestyle changes needed. If additional interventions were performed, regular follow-ups may be necessary to monitor vascular health and the effectiveness of the treatment.
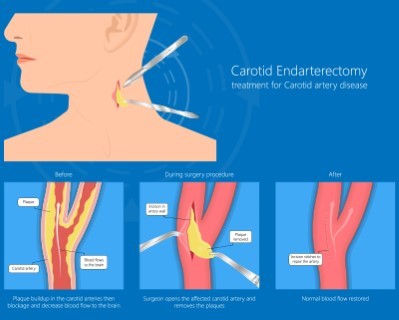
Carotid Angiography
- Purpose: Diagnoses blockages or narrowing in the carotid arteries, which supply blood to the brain.
- Procedure: A catheter is inserted into the carotid arteries, and contrast dye is injected to visualize the arteries on X-ray images.
Note: The information provided here applies to elective Carotid Angiography procedures without extraordinary circumstances. However, specifics may vary based on individual patient factors, such as the severity of carotid artery disease, the presence of other vascular conditions, or any complications that might arise during the procedure. The patient’s overall health, the need for additional interventions, or the complexity of the angiography can also influence the procedure and recovery process.
Inpatient/Outpatient
Carotid Angiography is typically performed as an outpatient procedure, allowing most patients to return home the same day. However, if the procedure reveals significant blockages that require immediate intervention, or if complications arise, a hospital stay might be necessary for further treatment and observation.Hospital Stay Duration
Most patients undergoing Carotid Angiography are monitored for a few hours after the procedure and can usually be discharged on the same day. If additional treatments, such as carotid stenting or surgery, are performed during the same session, an overnight stay might be required to ensure the patient’s condition remains stable.Type of Anesthesia
The procedure is usually performed under local anesthesia at the catheter insertion site, typically in the groin or arm. Mild sedation may also be administered to help the patient relax during the procedure. General anesthesia is rarely used but may be considered in specific cases, depending on the patient’s condition and the complexity of the procedure.Travel After Procedure
Patients are generally advised to avoid travel for at least 24 hours after Carotid Angiography, particularly if sedation was used. Depending on the findings and any additional procedures performed, longer or more strenuous travel may be postponed for a few days to ensure the patient is stable and comfortable.Pre-procedure Preparation
Before the procedure, patients are typically instructed to fast for several hours. They may also need to temporarily stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to reduce the risk of bleeding during the procedure.Procedure Duration
Carotid Angiography usually takes about 1 to 2 hours, depending on the complexity of the case and whether any additional interventions are needed during the procedure.Recovery Time
Most patients can resume light activities within a day or two after the procedure. However, it is recommended to avoid strenuous activities for several days, particularly those that could put stress on the catheter insertion site.Estimated Cost
The cost of Carotid Angiography can vary depending on the hospital, geographic location, and whether any additional procedures, such as stenting or surgery, are performed. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care involves monitoring the catheter insertion site for signs of infection, bleeding, or swelling. Patients will also need to follow up with their healthcare provider to review the results of the angiography and discuss any further treatment or lifestyle changes needed. If additional interventions were performed, regular follow-ups may be necessary to monitor vascular health and the effectiveness of the treatment.

Carotid Artery Stenting
- Purpose: Treats narrowing or blockages in the carotid arteries to prevent strokes.
- Procedure: A stent is placed in the carotid artery via a catheter to keep the artery open and maintain blood flow to the brain.
-
Note: The information provided here applies to elective Carotid Artery Stenting procedures without extraordinary circumstances. However, specifics may vary based on individual patient factors, such as the severity of carotid artery disease, the presence of other vascular conditions, or any complications that might arise during the procedure. The patient’s overall health, the complexity of the stenting process, and any additional interventions required can also influence the procedure and recovery process.
Inpatient/Outpatient
Carotid Artery Stenting is typically performed as an inpatient procedure. This approach allows for close monitoring before, during, and after the procedure to ensure the stent is properly placed and that the patient's condition is stable. Most patients will require a hospital stay for observation to manage any potential complications, such as bleeding, stroke, or changes in heart rhythm.Hospital Stay Duration
Patients undergoing Carotid Artery Stenting usually stay in the hospital for 1 to 2 days. This hospital stay ensures that the stent is functioning correctly and that there are no immediate complications. Longer stays may be required if the patient has other underlying conditions or if additional interventions are needed.Type of Anesthesia
The procedure is typically performed under local anesthesia at the catheter insertion site, usually in the groin, combined with mild sedation to keep the patient comfortable. General anesthesia is rarely used, but it may be considered in specific cases depending on the patient’s condition and the complexity of the procedure.Travel After Procedure
Patients are generally advised to avoid travel for at least a few days after Carotid Artery Stenting, particularly if sedation was used or if there are concerns about the stability of the stent. It’s important to follow the healthcare provider’s specific recommendations regarding travel and activity levels post-procedure.Pre-procedure Preparation
Before the procedure, patients are usually instructed to fast for several hours. They may also need to temporarily stop certain medications, particularly blood thinners, as directed by their healthcare provider to reduce the risk of bleeding during the procedure. Pre-procedure imaging and assessments are often conducted to plan the stenting process effectively.Procedure Duration
The Carotid Artery Stenting procedure typically takes about 1 to 2 hours, though the duration can vary depending on the complexity of the case and whether any additional interventions are required.Recovery Time
Most patients can begin to resume light activities within a week, though full recovery may take several weeks. It is crucial to avoid strenuous activities during the initial recovery period and to adhere to the healthcare provider’s instructions on managing the stent and overall vascular health.Estimated Cost
The cost of Carotid Artery Stenting can vary widely depending on the hospital, geographic location, and the specifics of the patient’s condition. For detailed cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care involves monitoring the stent and the incision site for signs of complications, such as infection, bleeding, or swelling. Patients will need to attend follow-up appointments to assess the success of the procedure and to discuss any necessary lifestyle changes or further treatment. Long-term follow-up is essential to monitor the patency of the stent and overall vascular health.
-closure_20240716230705769875__0.webp)
Atrial Septal Defect (ASD) Closure
- Purpose: Closes a hole in the heart wall (septum) between the atria.
- Procedure: A closure device is delivered through a catheter and deployed to seal the defect.
-
Note: The information provided here applies to elective Atrial Septal Defect (ASD) Closure procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the size and location of the defect, the presence of other heart conditions, or any complications that might arise during the procedure. The patient’s overall health, the complexity of the defect, and any additional cardiac interventions required can also influence the procedure and recovery process.
Inpatient/Outpatient
ASD Closure is typically performed as an inpatient procedure. Given the nature of the intervention and the importance of monitoring heart function, most patients are admitted to the hospital for at least one night for observation. This allows the healthcare team to closely monitor the patient’s heart rhythm and ensure the closure device or surgical repair is functioning properly.Hospital Stay Duration
Patients undergoing ASD Closure usually stay in the hospital for 1 to 3 days. This hospital stay allows for careful monitoring to ensure that the defect is properly closed and that there are no immediate complications, such as arrhythmias, bleeding, or device-related issues. Some patients, particularly those with other underlying conditions, may require a longer stay for additional observation.Type of Anesthesia
The procedure is typically performed under general anesthesia, especially when the closure is done via catheter-based methods or open-heart surgery. General anesthesia ensures that the patient is completely unconscious and does not experience any discomfort during the procedure.Travel After Procedure
Patients are generally advised to avoid travel for at least a week after the procedure, particularly if general anesthesia was used or if the patient underwent open-heart surgery. It is crucial to allow time for initial recovery and to ensure that there are no early complications. The healthcare provider will provide specific recommendations based on the patient’s recovery progress.Pre-procedure Preparation
Prior to the procedure, patients are usually instructed to fast for several hours. They may also undergo a series of pre-procedure tests, including echocardiograms and blood work, to ensure they are good candidates for ASD Closure. Adjustments to medications, especially blood thinners, may also be required to reduce the risk of bleeding during the procedure.Procedure Duration
The duration of the ASD Closure procedure can vary, typically lasting between 1 to 3 hours, depending on the method used (catheter-based vs. surgical) and the complexity of the defect.Recovery Time
Recovery time varies depending on the method of closure. For catheter-based closures, most patients can return to light activities within a week, although full recovery may take a few weeks. For open-heart surgery, recovery is more extensive, often taking several weeks to a few months. Patients should follow their healthcare provider’s instructions regarding activity levels and any necessary lifestyle adjustments post-procedure.Estimated Cost
The cost of ASD Closure can vary significantly depending on the hospital, geographic location, and the specifics of the procedure. Catheter-based closures typically differ in cost from surgical repairs. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care includes monitoring the patient for any signs of complications, such as arrhythmias, infection, or device-related issues (in the case of catheter-based closures). Follow-up appointments are essential to assess the success of the closure and to monitor heart function over time. Patients will also receive guidance on activity restrictions and any necessary medications to support recovery.
-closure_20240716230747928374__0.webp)
Patent Foramen Ovale (PFO) Closure
- Purpose: Closes a small hole in the heart wall that didn’t close naturally after birth.
- Procedure: Similar to ASD closure, a closure device is placed to seal the PFO.
-
Note: The information provided here applies to elective Patent Foramen Ovale (PFO) Closure procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the size of the PFO, the presence of other heart or vascular conditions, or any complications that might arise during the procedure. The patient’s overall health, the complexity of the closure, and the need for additional cardiac interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
PFO Closure is typically performed as an inpatient procedure. Most patients are admitted to the hospital for at least one night following the procedure to allow for close monitoring of heart function and to ensure the closure device or surgical repair is functioning properly. This monitoring is crucial to detect any immediate complications, such as arrhythmias or issues with the closure device.Hospital Stay Duration
Patients undergoing PFO Closure usually stay in the hospital for 1 to 2 days. This stay allows the healthcare team to monitor the heart and ensure there are no immediate complications, such as bleeding, arrhythmias, or device-related issues. In some cases, particularly if the patient has other underlying health conditions, a longer stay may be necessary for additional observation.Type of Anesthesia
The procedure is typically performed under general anesthesia, especially when the closure is done via a catheter-based method. General anesthesia ensures that the patient is unconscious and does not experience any discomfort during the procedure. In some cases, conscious sedation may be used depending on the method and the patient’s condition.Travel After Procedure
Patients are generally advised to avoid travel for at least a week after the procedure, particularly if general anesthesia was used. This allows time for initial recovery and ensures that there are no early complications. The healthcare provider will provide specific recommendations based on the patient’s recovery progress.Pre-procedure Preparation
Before the procedure, patients are usually instructed to fast for several hours. They may also undergo a series of pre-procedure tests, including echocardiograms and blood work, to ensure they are suitable candidates for PFO Closure. Adjustments to medications, particularly blood thinners, may also be necessary to minimize the risk of bleeding during the procedure.Procedure Duration
The PFO Closure procedure typically lasts between 1 to 2 hours, depending on the method used (catheter-based vs. surgical) and the complexity of the defect.Recovery Time
Recovery time varies depending on the method of closure. For catheter-based closures, most patients can return to light activities within a week, though full recovery may take a few weeks. For surgical repairs, recovery is more extensive and may take several weeks to a few months. Patients should follow their healthcare provider’s instructions regarding activity levels and any necessary lifestyle adjustments post-procedure.Estimated Cost
The cost of PFO Closure can vary depending on the hospital, geographic location, and the specifics of the procedure. Catheter-based closures typically differ in cost from surgical repairs. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care includes monitoring the patient for signs of complications, such as arrhythmias, infection, or device-related issues (in the case of catheter-based closures). Follow-up appointments are essential to assess the success of the closure and to monitor heart function over time. Patients will also receive guidance on activity restrictions and any necessary medications to support recovery.
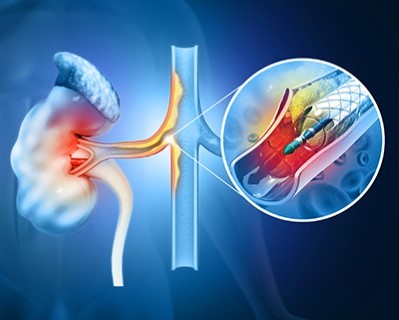
Renal Artery Angioplasty and Stenting
- Purpose: Treats narrowing of the arteries supplying the kidneys to improve blood flow and kidney function.
- Procedure: A balloon catheter and stent are used to open the narrowed renal artery.
-
Note: The information provided here applies to elective Renal Artery Angioplasty and Stenting procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the severity of renal artery stenosis, the presence of other vascular conditions, or any complications that might arise during the procedure. The patient’s overall health, the complexity of the stenting process, and any additional interventions required can also influence the procedure and recovery process.
Inpatient/Outpatient
Renal Artery Angioplasty and Stenting is typically performed as an inpatient procedure. This allows for close monitoring before, during, and after the procedure to ensure that the stent is properly placed and that the patient's condition is stable. Most patients will require a hospital stay for observation to manage any potential complications, such as bleeding, changes in kidney function, or blood pressure fluctuations.Hospital Stay Duration
Patients undergoing Renal Artery Angioplasty and Stenting usually stay in the hospital for 1 to 2 days. This stay ensures that the procedure was successful and that there are no immediate complications. Patients with complex conditions or who require additional interventions may need a longer hospital stay for further observation and care.Type of Anesthesia
The procedure is typically performed under local anesthesia at the catheter insertion site, often in the groin, combined with mild sedation to keep the patient comfortable. General anesthesia is rarely used, but may be considered in specific cases depending on the patient’s condition and the complexity of the procedure.Travel After Procedure
Patients are generally advised to avoid travel for at least a few days after Renal Artery Angioplasty and Stenting, particularly if sedation was used or if there are concerns about the stability of the stent. It’s important to follow the healthcare provider’s specific recommendations regarding travel and activity levels post-procedure.Pre-procedure Preparation
Before the procedure, patients are usually instructed to fast for several hours. They may also need to temporarily stop certain medications, particularly blood thinners, as directed by their healthcare provider to reduce the risk of bleeding during the procedure. Pre-procedure imaging and assessments are often conducted to plan the angioplasty and stenting process effectively.Procedure Duration
The Renal Artery Angioplasty and Stenting procedure typically takes about 1 to 2 hours, though the duration can vary depending on the complexity of the case and whether any additional interventions are required.Recovery Time
Most patients can begin to resume light activities within a week, though full recovery may take several weeks. It is crucial to avoid strenuous activities during the initial recovery period and to adhere to the healthcare provider’s instructions on managing the stent and overall vascular health.Estimated Cost
The cost of Renal Artery Angioplasty and Stenting can vary widely depending on the hospital, geographic location, and the specifics of the patient’s condition. For detailed cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care involves monitoring the stent and the catheter insertion site for signs of complications, such as infection, bleeding, or swelling. Patients will need to attend follow-up appointments to assess the success of the procedure and to discuss any necessary lifestyle changes or further treatment. Long-term follow-up is essential to monitor kidney function and the patency of the stent.
-procedure_20240720234856220384__0.webp)
Mitral Valve Clip (MitraClip) Procedure
- Purpose: Treats mitral regurgitation by clipping together parts of the mitral valve to reduce leakage.
- Procedure: A catheter-based device is used to place the clip on the mitral valve.
-
Note: The information provided here applies to elective Mitral Valve Clip (MitraClip) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the severity of mitral regurgitation, the presence of other heart conditions, or any complications that might arise during the procedure. The patient’s overall health, the complexity of the valve repair, and any additional interventions required can also influence the procedure and recovery process.
Inpatient/Outpatient
The Mitral Valve Clip (MitraClip) procedure is typically performed as an inpatient procedure. Due to the complexity of the intervention and the need for detailed monitoring of heart function, most patients are admitted to the hospital for at least one night following the procedure. This allows the healthcare team to ensure the MitraClip is properly positioned and that the patient’s condition remains stable.Hospital Stay Duration
Patients undergoing the Mitral Valve Clip procedure usually stay in the hospital for 1 to 3 days. This stay allows for close monitoring of heart function and the MitraClip’s performance, as well as the management of any potential complications, such as bleeding, arrhythmias, or issues with the clip placement. In some cases, particularly for patients with other underlying conditions, a longer stay may be necessary for further observation.Type of Anesthesia
The procedure is typically performed under general anesthesia to ensure the patient is fully unconscious and comfortable during the intervention. This is important as the procedure involves precise manipulation of the heart’s mitral valve, and general anesthesia helps minimize patient movement and discomfort.Travel After Procedure
Patients are generally advised to avoid travel for at least a week after the procedure, particularly if general anesthesia was used. This allows time for initial recovery and ensures that there are no early complications. The healthcare provider will provide specific recommendations based on the patient’s recovery progress.Pre-procedure Preparation
Before the procedure, patients are usually instructed to fast for several hours. They may also undergo a series of pre-procedure tests, including echocardiograms, blood work, and possibly a cardiac catheterization, to ensure they are good candidates for the MitraClip procedure. Adjustments to medications, particularly blood thinners, may also be required to minimize the risk of bleeding during the procedure.Procedure Duration
The Mitral Valve Clip procedure typically lasts between 2 to 4 hours, depending on the complexity of the valve regurgitation and the specific conditions of the patient’s heart.Recovery Time
Recovery time varies, but most patients can return to light activities within a week. Full recovery, including a return to more strenuous activities, may take several weeks, depending on the patient’s overall health and how well they respond to the procedure. Patients should follow their healthcare provider’s instructions regarding activity levels and any necessary lifestyle adjustments post-procedure.Estimated Cost
The cost of the Mitral Valve Clip procedure can vary significantly depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care includes monitoring the patient for any signs of complications, such as arrhythmias, infection, or issues with the MitraClip. Regular follow-up appointments are essential to assess the success of the procedure and to monitor heart function over time. Patients will also receive guidance on activity restrictions, medication management, and any necessary lifestyle changes to support their recovery and long-term heart health.
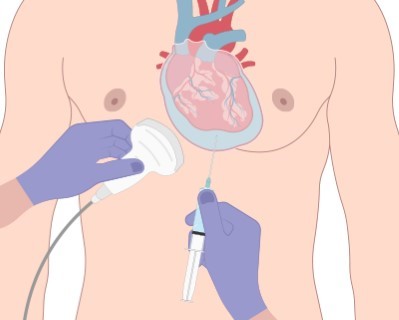
Pericardiocentesis
- Purpose: Removes excess fluid from the pericardial sac around the heart to relieve pressure.
- Procedure: A needle and catheter are used to aspirate the fluid from the pericardium.
-
Note: The information provided here applies to elective Pericardiocentesis procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the underlying cause of pericardial effusion, the presence of other heart or systemic conditions, or any complications that might arise during the procedure. The patient’s overall health, the amount of fluid to be drained, and the need for additional interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
Pericardiocentesis is typically performed as an inpatient procedure, especially when it is done to treat significant pericardial effusion that is causing symptoms such as shortness of breath or chest pain. The procedure may require close monitoring to ensure that the fluid drainage is effective and that the patient’s condition stabilizes afterward. In some cases, depending on the underlying cause and patient condition, it might be performed as an outpatient procedure with a short observation period.Hospital Stay Duration
Patients undergoing Pericardiocentesis usually stay in the hospital for 1 to 2 days. This allows for close monitoring to ensure that the effusion has been effectively drained and that there are no immediate complications, such as bleeding, infection, or recurrence of fluid accumulation. If the procedure was performed due to an emergency or if the patient has other underlying conditions, a longer stay may be required.Type of Anesthesia
The procedure is generally performed under local anesthesia to numb the area where the needle or catheter will be inserted. In some cases, mild sedation may be used to help the patient relax. General anesthesia is typically not required unless the procedure is particularly complex or if it is part of a larger surgical intervention.Travel After Procedure
Patients are generally advised to avoid travel for at least a few days after the procedure to ensure that they are stable and that there are no early complications, such as reaccumulation of fluid or infection. The healthcare provider will provide specific recommendations based on the patient’s recovery progress.Pre-procedure Preparation
Before the procedure, patients are usually instructed to fast for several hours. They may also need to undergo imaging tests, such as an echocardiogram, to assess the amount of fluid and to guide the procedure. Medications, particularly blood thinners, may need to be adjusted to reduce the risk of bleeding during the procedure.Procedure Duration
The Pericardiocentesis procedure typically takes about 30 minutes to 1 hour, depending on the amount of fluid being drained and the complexity of the case.Recovery Time
Most patients can resume light activities within a few days, but full recovery may take a week or more, depending on the underlying cause of the effusion and the patient’s overall health. Patients should follow their healthcare provider’s instructions regarding activity levels and any necessary follow-up care.Estimated Cost
The cost of Pericardiocentesis can vary depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care involves monitoring the patient for any signs of complications, such as infection at the insertion site, reaccumulation of fluid, or changes in heart function. Regular follow-up appointments are essential to assess the success of the procedure and to monitor for any recurrence of symptoms. Patients will also receive instructions on how to care for the insertion site and any restrictions on activities during recovery.
